Hypoglycemia is a critical medical condition characterized by abnormally low blood sugar levels. While it is a common concern for individuals with diabetes, it can also affect those without the condition under certain circumstances.
In this comprehensive guide, we will explore the various aspects of hypoglycemia, including its definition, symptoms, causes, management, and the specific impact of medications like beta blockers.
What is hypoglycemia?
Hypoglycemia, often referred to as low blood sugar, occurs when the concentration of glucose (sugar) in the blood falls below normal levels. The normal range for blood glucose levels typically hovers between 70 to 110 milligrams per deciliter (mg/dL).
Hypoglycemia is usually recognized when blood sugar drops below 70 mg/dL. Understanding what hypoglycemia is forms the foundation for effectively managing and preventing its occurrence.
Symptoms of hypoglycemia
Hypoglycemia, often referred to as low blood sugar, is a medical condition that demands prompt recognition and intervention. The symptoms of hypoglycemia can manifest differently from one individual to another, but understanding these warning signs is crucial for timely and effective management.
In this section, we will delve deeper into the various symptoms of hypoglycemia, shedding light on the mechanisms behind each symptom and their impact on daily life.
- Shakiness or Nervousness
- Sweating
- Chills and Clamminess
- Rapid Heartbeat
- Dizziness or Light-headedness
- Hunger and Nausea
- Irritability or Moodiness
- Confusion or Difficulty Concentrating
- Blurred Vision
- Seizures or Loss of Consciousness (in Severe Cases)
1. Shakiness or Nervousness
One of the most recognizable and immediate symptoms of hypoglycemia is shakiness or nervousness. This sensation is often experienced as a trembling or quivering feeling, typically in the hands and legs.
Mechanism
When blood sugar levels drop, the brain perceives it as a threat to the body’s energy supply. In response, the body releases stress hormones like adrenaline. This surge in adrenaline can lead to physical symptoms such as shakiness and a heightened sense of nervousness.
Impact
Shakiness and nervousness can interfere with daily activities and tasks, making it challenging to perform fine motor skills or concentrate on work or personal matters.
2. Sweating
Profuse sweating, even in cooler environments or without physical exertion, is a common symptom of hypoglycemia.
Mechanism
Sweating is another physiological response to low blood sugar levels. It is triggered by the release of stress hormones like adrenaline, which can lead to an increase in perspiration.
Impact
Excessive sweating can be uncomfortable and distressing, leading to a feeling of clamminess and the need to change clothing more frequently.
3. Chills and Clamminess
People experiencing hypoglycemia often report feeling cold and clammy to the touch.
Mechanism
The sensation of coldness and clamminess is a result of the body’s response to hypoglycemia-induced stress hormones. These hormones can constrict blood vessels, redirecting blood flow away from the skin’s surface to preserve warmth in the core.
Impact
These physical sensations can be disconcerting and uncomfortable, making individuals with hypoglycemia feel uneasy and out of sorts.
4. Rapid Heartbeat
An increased heart rate is a common physiological response to low blood sugar levels.
Mechanism
When blood sugar drops, the body perceives it as a stressor, prompting the release of adrenaline. This hormone elevates heart rate and prepares the body for a “fight or flight” response.
Impact
While a rapid heartbeat is a protective response, it can be alarming to the individual experiencing it. It may contribute to feelings of anxiety and discomfort.
5. Dizziness or Light-headedness
Individuals with hypoglycemia may experience dizziness or light-headedness, feeling unsteady or on the verge of fainting.
Mechanism
Low blood sugar levels can affect brain function, leading to dizziness and an unsteady feeling. The brain relies on a steady supply of glucose for proper functioning, and when that supply is compromised, it can result in these sensations.
Impact
Dizziness and light-headedness can significantly impair one’s ability to carry out everyday activities safely.
6. Hunger and Nausea
An intense craving for food is a common symptom of hypoglycemia, often accompanied by nausea.
Mechanism
As blood sugar levels decline, the body sends signals to the brain, indicating a need for more energy. This signal is perceived as intense hunger and, in some cases, can lead to nausea as the body attempts to redirect energy away from the digestive system.
Impact
The combination of hunger and nausea can be distressing and interfere with an individual’s ability to focus or complete tasks.
7. Irritability or Moodiness
Sudden changes in mood or temperament, including irritability and mood swings, can be indicative of hypoglycemia.
Mechanism
Low blood sugar levels can disrupt the brain’s neurotransmitter balance, leading to mood disturbances. The stress response triggered by hypoglycemia can also contribute to feelings of irritability.
Impact
Mood swings and irritability can strain personal and professional relationships and hinder effective communication.
8. Confusion or Difficulty Concentrating
Cognitive impairment, such as confusion and difficulty concentrating, is a common symptom of hypoglycemia.
Mechanism
The brain relies on glucose as its primary energy source. When blood sugar levels drop, the brain may struggle to function optimally, leading to cognitive deficits.
Impact
Confusion and difficulty concentrating can be particularly worrisome, as they affect an individual’s ability to make informed decisions and carry out tasks safely.
9. Blurred Vision
Visual disturbances, including blurred vision or experiencing double vision, can occur during episodes of hypoglycemia.
Mechanism
Low blood sugar can affect the functioning of the eyes and the optic nerves, leading to visual disturbances.
Impact
Impaired vision can be dangerous, especially when individuals need to operate vehicles or machinery.
10. Seizures or Loss of Consciousness (in Severe Cases)
In extreme instances of hypoglycemia, individuals may experience seizures or lose consciousness.
Mechanism
Severe hypoglycemia deprives the brain of the glucose it needs to function, which can lead to convulsions or unconsciousness.
Impact
Seizures and loss of consciousness are medical emergencies requiring immediate intervention and medical attention.
Medications / disorders that can cause hypoglycemia
Some medications that are used to treat diabetes have a higher risk of causing hypoglycemia especially if the medication is taken without food. It can result from various factors, including medications and underlying health conditions. Below are those medications:
- Insulin
- Glipizide / glimepiride / glyburide
- Nateglinide / repaglinide
- Pramlintide
Other disorders or medications that can cause hypoglycemia include:
- Excessive alcohol consumption
- Severe hepatitis
- Beta blockers (metoprolol, atenolol, carvedilol, etc): not only beta blockers may cause hypoglycemia, they can also mask certain symptoms such as shakiness, palpitation, and anxiety. Sweating and hunger are not masked.
- Ciprofloxacin / levofloxacin
Insulin
Insulin is a hormone used in diabetes management, especially for individuals with type 1 diabetes. However, if insulin dosage is not adjusted correctly or if there is an overdose, it can lead to a rapid drop in blood sugar levels.
Glipizide/Glimepiride/Glyburide
These are common medications prescribed to individuals with type 2 diabetes. They work by stimulating the pancreas to produce more insulin. However, if not taken as directed, they can cause excessive insulin production, leading to hypoglycemia.
Nateglinide/Repaglinide
These medications, known as meglitinides, are used to stimulate insulin secretion in individuals with type 2 diabetes. Similar to sulfonylureas, they can lead to excessive insulin production if not dosed correctly.
Pramlintide
Pramlintide is an injectable medication used in diabetes management. It works by slowing down gastric emptying and suppressing appetite. While it is effective for blood sugar control, it can also lead to hypoglycemia if not used as prescribed.
Excessive Alcohol Consumption
Alcohol, when consumed in excess, can interfere with the liver’s ability to release glucose into the bloodstream. This can lead to a sudden drop in blood sugar levels, especially in individuals with diabetes.
Severe Hepatitis
Hepatitis, particularly in severe cases, can affect liver function. The liver plays a crucial role in regulating blood sugar levels by releasing glucose when needed. Hepatitis-induced liver dysfunction can disrupt this process, contributing to hypoglycemia.
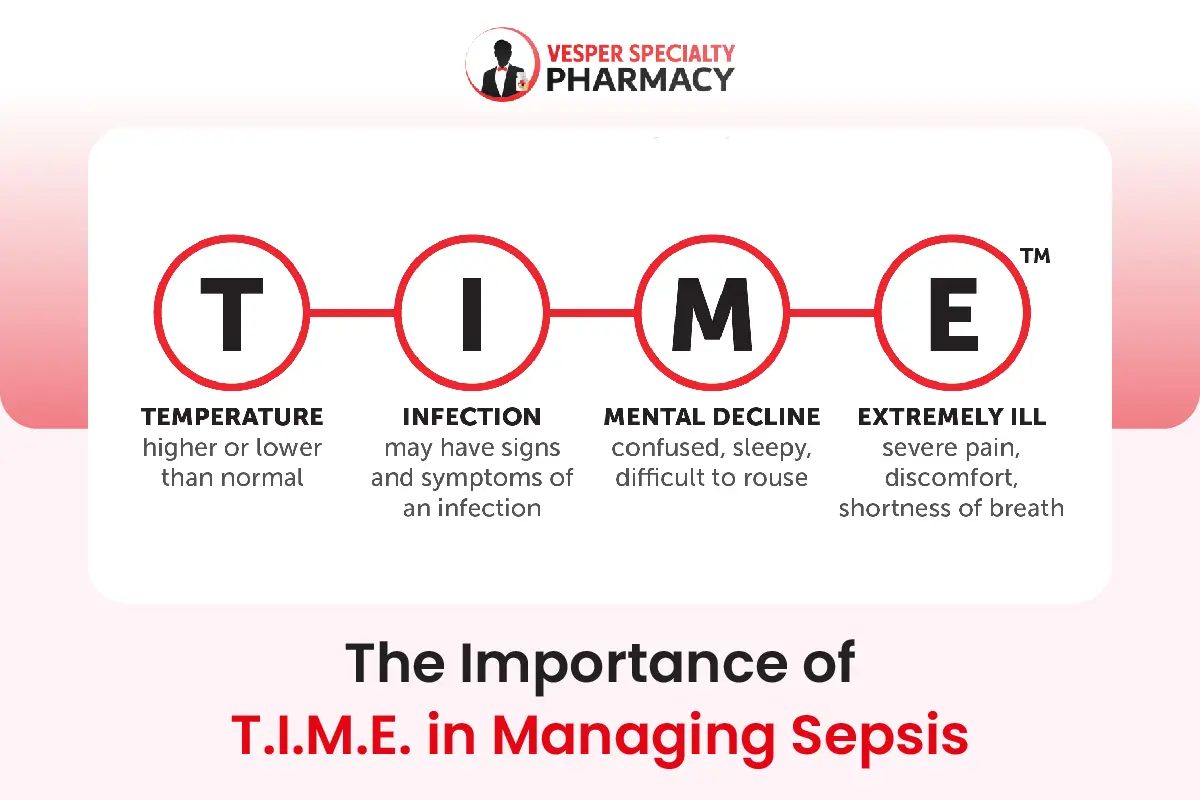
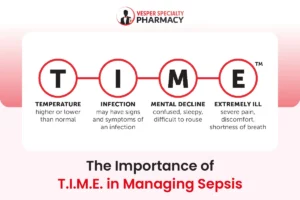
Beta Blockers (Metoprolol, Atenolol, Carvedilol)
Beta-blockers are commonly prescribed for conditions like hypertension and heart disease. While they don’t directly cause hypoglycemia, they can mask its symptoms, making it challenging for individuals to recognize low blood sugar levels.
Ciprofloxacin/Levofloxacin
These antibiotics have been associated with rare cases of hypoglycemia. While the mechanism isn’t fully understood, it’s essential to be aware of this potential side effect when taking these medications.
How to treat hypoglycemia
Managing and treating hypoglycemia is crucial to prevent it from progressing into a severe and potentially life-threatening condition. Here’s a step-by-step guide:
Step 1: Check Blood Sugar Levels
When you experience symptoms of hypoglycemia, it’s essential to confirm your blood sugar levels. You can use a glucose meter to do this quickly. If your reading is below 70 mg/dL, you need to take action.
Step 2: Consume 15-20 Grams of Fast-Acting Carbohydrates
The first line of treatment for hypoglycemia is to consume fast-acting carbohydrates. These are substances that raise blood sugar levels quickly. Examples include:
- Glucose Tablets: These are designed specifically for raising blood sugar and are readily available at pharmacies.
- Fruit Juice: Orange juice or apple juice can work effectively.
- Regular (Not Diet) Soda: The sugar content in regular soda can help boost blood sugar.
- Candy: Non-chocolate candies like jelly beans or hard candies can be used.
The “Rule of 15” is a common guideline to follow during this step. It involves consuming 15-20 grams of fast-acting carbohydrates and then waiting for 15 minutes to recheck your blood sugar
15 grams of glucose or simple carbohydrates





Step 3: Recheck Blood Sugar After 15 Minutes
After consuming the fast-acting carbohydrates, it’s essential to monitor your blood sugar levels closely. After 15 minutes, check your blood sugar again. If it remains below the target range (usually below 70 mg/dL), repeat the intake of fast-acting carbohydrates.
Step 4: Eat a Snack or Meal
Once your blood sugar has returned to a normal range and you’re feeling better, it’s important to have a small snack or meal to stabilize your blood sugar levels. This helps prevent another drop in blood sugar.
Glucagon
Glucagon is recommended to be prescribed for all diabetic patients at increased risk of severe hypoglycemia. It is only used when the patient is not conscious enough to treat. Caregivers, school personnel, or family members of these patients should be trained on when and how to administer glucagon. Carbohydrates should be administered as soon as possible after glucagon. It is important to note that glucagon will not work for patients with alcohol-induced due to depleted glycogen stores in those individuals. If no response to glucagon, IV dextrose may need to be administered.
Administration
Place patient lying sideways to prevent choking upon return to consciousness. Mix powder for injection by adding 1 mL of manufacturer-supplied sterile diluent or sterile water for injection to a vial containing 1 unit of the drug, to provide solutions containing 1 mg of glucagon/mL. Shake vial gently to dissolve. Use
Frequently Asked Questions
Who treats hypoglycemia?
Hypoglycemia is often managed by the individual experiencing it, especially if they have diabetes. However, severe cases may require medical attention from primary care physicians, endocrinologists, or in emergencies, hospital staff.
What Medication is used for hypoglycemia?
The primary treatment for hypoglycemia is the intake of fast-acting carbohydrates. In severe cases, glucagon injections are used, which can be administered by another person if the individual is unable or unconscious.
Management of hypoglycemia?
Continuous monitoring and management strategies, such as regular blood sugar checks and carrying fast-acting carbohydrates, are crucial. Educating friends and family about how to assist in an emergency is also important.
Can beta blockers cause hypoglycemia?
Beta-blockers themselves don’t typically cause hypoglycemia but can mask its symptoms, making it harder to recognize and treat promptly.
Beta blockers and hypoglycemia?
Beta-blockers can interfere with the natural adrenaline response to hypoglycemia, which can suppress symptoms like tremors, palpitations, and anxiety, delaying awareness of low blood sugar.
How do beta blockers cause hypoglycemia?
While beta-blockers do not directly cause hypoglycemia, their impact on hypoglycemia awareness and potential interference with glycogenolysis (the breakdown of glycogen to glucose) in the liver can complicate blood sugar management.
Why do beta blockers cause hypoglycemia?
Beta-blockers can prolong hypoglycemia by impairing the body’s natural response to low blood sugar. They can also mask the adrenergic symptoms (like tremors and palpitations), which are early warning signs of hypoglycemia.
Conclusion
Episodes of hypoglycemia are dangerous for patients. They decrease
References
- Cryer PE, Davis SN. Hypoglycemia. In: Jameson J, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J. eds. Harrison’s Principles of Internal Medicine, 20e New York, NY: McGraw-Hill; . http://nv-ezproxy.roseman.edu:2759/content.aspx?bookid=2129§ionid=192288656. Accessed February 25, 2019.
- American Diabetes Association. 6. Glycemic targets: Standards of Medical Care in Diabetes 2019. Diabetes Care 2019;42(Suppl. 1):S61–S70.