The pancreas plays a pivotal role in maintaining overall health and well-being through its diverse functions as both an endocrine and exocrine gland. Its ability to regulate blood sugar levels, facilitate digestion, and support metabolic processes underscores its critical importance in the body’s functioning. However, pancreatic diseases such as pancreatitis, pancreatic cancer, and diabetes mellitus can pose significant challenges to health and quality of life.
Table of Contents
Definition of the Pancreas
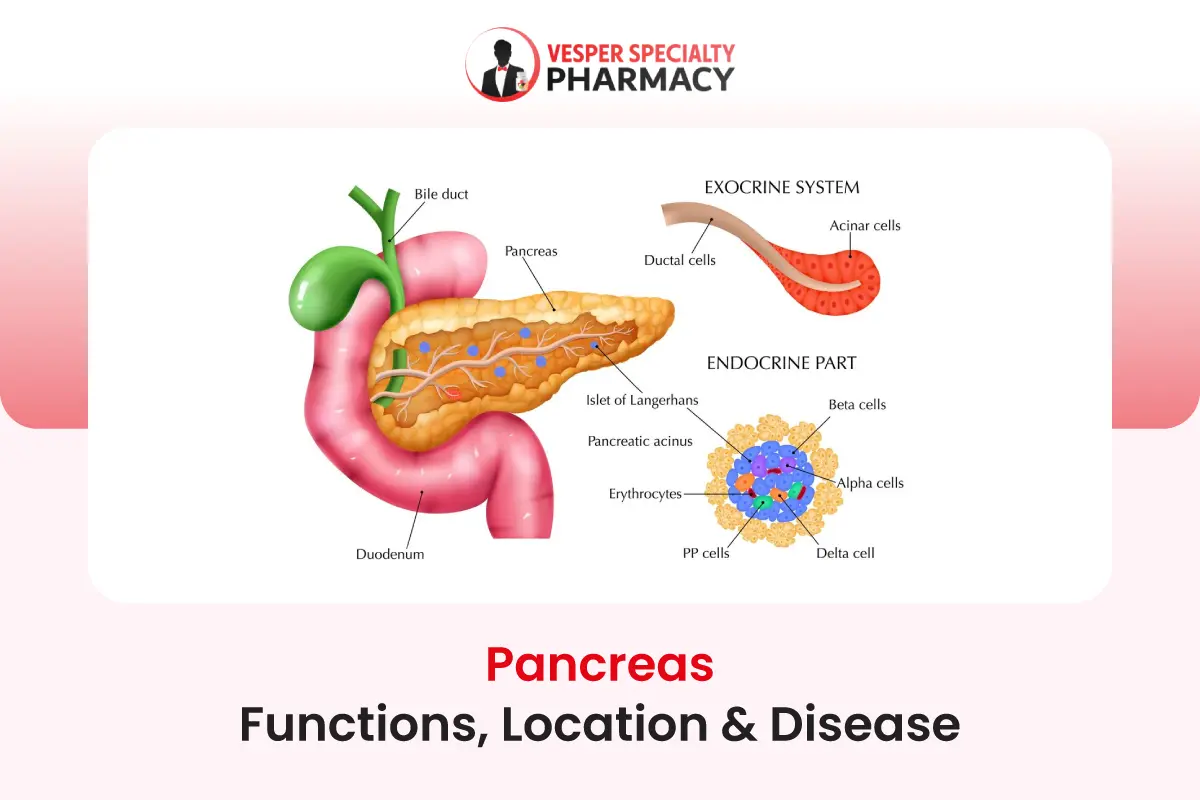
The pancreas is a vital organ located in the abdominal cavity, nestled behind the stomach and adjacent to the small intestine. It serves a dual role in the body, functioning both as an endocrine gland and an exocrine gland. Structurally, the pancreas is elongated and resembles a flattened fish, with its head tucked into the curve of the duodenum, the first part of the small intestine.
Importance of the Pancreas in the Body’s Functioning
The pancreas plays a crucial role in maintaining the body’s overall health and functioning. Its diverse functions contribute significantly to various physiological processes, including digestion, metabolism, and blood sugar regulation.
Digestive Function
As an exocrine gland, the pancreas produces and secretes digestive enzymes into the small intestine. These enzymes, such as amylase, lipase, and proteases, break down carbohydrates, fats, and proteins from ingested food, facilitating their absorption and utilization by the body. Without adequate pancreatic enzyme production, proper digestion and nutrient absorption are compromised, leading to malnutrition and related health issues.
Endocrine Function
In addition to its role in digestion, the pancreas serves as an endocrine gland, releasing hormones directly into the bloodstream to regulate various metabolic processes. The two primary hormones produced by specialized clusters of cells within the pancreas are insulin and glucagon.
Insulin
Produced by beta cells in the pancreas, insulin plays a central role in regulating blood sugar levels by facilitating the uptake of glucose from the bloodstream into cells, where it is utilized for energy production or stored for future use. Insulin helps maintain stable blood glucose concentrations, preventing hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar), both of which can have detrimental effects on health if left uncontrolled.
Glucagon
Secreted by alpha cells in the pancreas, glucagon acts in opposition to insulin, helping to raise blood sugar levels when they fall too low. Glucagon stimulates the breakdown of glycogen stored in the liver into glucose, which is then released into the bloodstream to provide a readily available source of energy for the body’s cells.
Anatomy of the Pancreas
Venous drainage from the pancreas is facilitated by the pancreatic veins, which ultimately drain into the portal vein, directing blood from the digestive organs to the liver for processing and detoxification before returning to the heart. This intricate network of blood vessels ensures adequate perfusion of the pancreas, supporting its physiological functions and metabolic demands.
Location within the Body
The pancreas is situated in the abdominal cavity, positioned horizontally across the posterior wall behind the stomach. It extends from the curvature of the duodenum, the first part of the small intestine, to the spleen on the left side of the abdomen. The pancreas is nestled between the stomach, small intestine, liver, and spleen, with its head located near the curvature of the duodenum, its body extending transversely behind the stomach, and its tail tapering towards the spleen.
Structure and Organization
Head
The head of the pancreas is the widest part of the organ and is nestled within the curvature of the duodenum.
It lies adjacent to the right side of the abdominal aorta and the superior mesenteric artery.
The bile duct, which carries bile from the liver and gallbladder, runs through the head of the pancreas before joining the pancreatic duct to form the ampulla of Vater, which empties into the duodenum.
Body
The body of the pancreas extends horizontally behind the stomach, spanning toward the left side of the abdomen.
It lies anterior to the aorta, left kidney, left adrenal gland, and left renal vessels.
The body of the pancreas is responsible for producing and secreting digestive enzymes and bicarbonate ions essential for digestion and neutralization of stomach acid.
Tail
The tail of the pancreas tapers towards the spleen on the left side of the abdomen.
It is nestled between the spleen and the left kidney.
The tail contains endocrine cell clusters known as the islets of Langerhans, which produce hormones such as insulin and glucagon involved in blood sugar regulation.
Blood Supply to the Pancreas
The pancreas receives its blood supply from branches of the celiac artery and the superior mesenteric artery, two major arteries originating from the abdominal aorta. These arteries branch into smaller vessels that supply oxygen-rich blood to the pancreatic tissue, ensuring its metabolic needs are met for proper functioning.
The arterial blood supply to the pancreas includes
- The pancreatic branches of the splenic artery, primarily supply the body and tail of the pancreas.
- The pancreaticoduodenal arteries arise from the gastroduodenal artery (a branch of the common hepatic artery) and the superior mesenteric artery. These arteries supply blood to the head and uncinate process of the pancreas, as well as the duodenum.
Functions of the Pancreas
The pancreas fulfills critical endocrine and exocrine functions essential for maintaining metabolic homeostasis, regulating blood sugar levels, and facilitating efficient digestion and nutrient absorption. Dysfunction or impairment of pancreatic function can lead to metabolic disorders, digestive complications, and systemic health issues, underscoring the pivotal role of the pancreas in overall physiological well-being.
Endocrine Functions
Production of Insulin
- The pancreas plays a crucial role in regulating blood sugar levels through the production and secretion of insulin.
- Insulin is synthesized and released by beta cells within specialized clusters known as the islets of Langerhans, primarily located in the pancreatic body and tail.
- Upon ingestion of carbohydrates, insulin secretion is stimulated in response to rising blood glucose levels.
- Insulin acts on target cells, particularly in the liver, muscle, and adipose tissue, to facilitate the uptake of glucose from the bloodstream into cells for energy production or storage.
- By promoting glucose uptake, insulin helps lower blood sugar levels, preventing hyperglycemia and maintaining metabolic homeostasis.
Production of Glucagon
- In addition to insulin, the pancreas produces and releases the hormone glucagon to regulate blood sugar levels.
- Glucagon is synthesized and secreted by alpha cells within the islets of Langerhans, predominantly located in the pancreatic body and tail.
- Glucagon secretion is stimulated when blood glucose levels drop, signaling a need to increase glucose availability for energy production.
- Glucagon acts on the liver to stimulate the breakdown of glycogen into glucose through a process known as glycogenolysis, thereby raising blood sugar levels.
- Additionally, glucagon promotes gluconeogenesis, the synthesis of glucose from non-carbohydrate sources such as amino acids and fatty acids, further contributing to blood sugar elevation.
Regulation of Blood Sugar Levels
- Through the coordinated action of insulin and glucagon, the pancreas maintains tight control over blood sugar levels, a process essential for overall metabolic health.
- Insulin and glucagon act in opposition to each other to ensure blood glucose concentrations remain within a narrow range, preventing hyperglycemia or hypoglycemia.
- This dynamic interplay between insulin and glucagon helps regulate glucose metabolism, providing cells with a steady supply of energy while preventing fluctuations in blood sugar that can lead to metabolic dysfunction and related complications.
Exocrine Functions
Production of Digestive Enzymes
- The pancreas serves as a vital exocrine gland, producing and secreting digestive enzymes essential for the breakdown of carbohydrates, fats, and proteins in ingested food.
- These digestive enzymes, including amylase (for carbohydrates), lipase (for fats), and various proteases (for proteins), are synthesized by pancreatic acinar cells located within the exocrine tissue of the pancreas.
- Upon stimulation by hormonal and neural signals triggered by food ingestion, pancreatic enzymes are released into the small intestine via the pancreatic duct, where they facilitate the digestion and absorption of nutrients.
Secretion of Bicarbonate Ions
- In addition to digestive enzymes, the pancreas secretes bicarbonate ions (HCO3-) into the small intestine to neutralize acidic chyme entering the stomach.
- Bicarbonate ions are produced and released by ductal cells within the pancreatic duct system, helping to maintain an optimal pH environment for enzymatic activity and efficient digestion.
- By neutralizing gastric acid, bicarbonate secretion from the pancreas contributes to the overall digestive process, protecting the intestinal mucosa from acidic damage and ensuring proper absorption of nutrients.
Role in Digestion
- The combined action of pancreatic enzymes and bicarbonate ions facilitates the digestion of carbohydrates, fats, and proteins within the small intestine, converting complex nutrients into absorbable forms.
- Pancreatic enzymes break down carbohydrates into simple sugars (e.g., glucose), fats into fatty acids and glycerol, and proteins into amino acids, peptides, and polypeptides.
- This breakdown of macronutrients by pancreatic enzymes enables their efficient absorption across the intestinal lining into the bloodstream, providing the body with essential nutrients necessary for growth, repair, and metabolic function.
Common Pancreatic Diseases
Common pancreatic diseases are crucial for early detection, timely intervention, and effective management to improve outcomes and quality of life for individuals affected by these conditions. Early recognition of symptoms, risk factors, and appropriate medical care are essential for optimizing treatment outcomes and minimizing complications associated with pancreatic diseases.
Pancreatitis
Pancreatitis refers to inflammation of the pancreas, which can be acute or chronic, each with distinct characteristics and clinical presentations.
Acute Pancreatitis
- Acute pancreatitis is a sudden onset inflammation of the pancreas, typically characterized by severe abdominal pain, nausea, vomiting, and elevated levels of pancreatic enzymes in the blood.
- Common causes of acute pancreatitis include gallstones, alcohol consumption, certain medications, infections, trauma, and metabolic disorders.
- Acute pancreatitis can range in severity from mild self-limiting episodes to severe cases with complications such as pancreatic necrosis, pseudocysts, and organ failure.
- Treatment for acute pancreatitis often involves hospitalization, intravenous fluids, pain management, and addressing the underlying cause to prevent a recurrence.
Chronic Pancreatitis
- Chronic pancreatitis is a progressive, long-term inflammation of the pancreas characterized by recurrent abdominal pain, digestive problems, and eventual loss of pancreatic function.
- Prolonged alcohol abuse is a leading cause of chronic pancreatitis, although other factors such as genetic predisposition, autoimmune conditions, and recurrent acute pancreatitis episodes can also contribute.
- Chronic pancreatitis leads to irreversible damage to pancreatic tissue, fibrosis, and impairment of exocrine and endocrine functions, resulting in malabsorption, diabetes, and nutritional deficiencies.
- Management of chronic pancreatitis focuses on pain relief, enzyme replacement therapy, nutritional support, and addressing complications such as diabetes and pancreatic pseudocysts.
Pancreatic Cancer
Pancreatic cancer is a malignant tumor that arises from the cells of the pancreas, often presenting late in its course with nonspecific symptoms and a poor prognosis.
- Pancreatic ductal adenocarcinoma is the most common type of pancreatic cancer, accounting for the majority of cases.
- Risk factors for pancreatic cancer include smoking, obesity, chronic pancreatitis, family history, and certain genetic syndromes.
- Symptoms of pancreatic cancer may include jaundice, abdominal pain, weight loss, fatigue, and digestive disturbances.
- Diagnosis typically involves imaging studies such as CT scans, MRI, endoscopic ultrasound, and biopsy for confirmation.
- Treatment options for pancreatic cancer depend on the stage of the disease and may include surgery, chemotherapy, radiation therapy, and targeted therapy.
Diabetes Mellitus
Diabetes mellitus is a group of metabolic disorders characterized by high blood sugar levels due to defects in insulin production, insulin action, or both.
Type 1 Diabetes
- Type 1 diabetes is an autoimmune condition in which the immune system attacks and destroys the insulin-producing beta cells in the pancreas.
- Individuals with type 1 diabetes require lifelong insulin therapy to regulate blood sugar levels and prevent complications.
- Symptoms of type 1 diabetes include excessive thirst, frequent urination, unexplained weight loss, fatigue, and blurred vision.
- Management of type 1 diabetes involves insulin therapy, blood sugar monitoring, dietary modifications, regular exercise, and careful monitoring for complications.
Type 2 Diabetes
- Type 2 diabetes is characterized by insulin resistance, where the body’s cells become resistant to the effects of insulin or the pancreas fails to produce enough insulin to meet the body’s demands.
- Risk factors for type 2 diabetes include obesity, sedentary lifestyle, family history, aging, and certain ethnicities.
- Symptoms of type 2 diabetes may develop gradually and include increased thirst, frequent urination, fatigue, blurred vision, and slow wound healing.
- Management of type 2 diabetes focuses on lifestyle modifications such as diet and exercise, oral medications to lower blood sugar levels, and in some cases, insulin therapy.
Other Pancreatic Disorders
Other pancreatic disorders include pancreatic cysts, pancreaticobiliary disorders, pancreatic neuroendocrine tumors (NETs), and hereditary pancreatitis, among others.
These disorders may present with a variety of symptoms and complications, requiring specialized diagnostic evaluation and management tailored to each case.
Diagnosis and Treatment
The diagnosis and treatment of pancreatic diseases involve a multidisciplinary approach, incorporating various diagnostic modalities and treatment strategies tailored to individual patient needs. Early diagnosis, timely intervention, and comprehensive care are essential for optimizing outcomes and improving the quality of life for individuals affected by pancreatic diseases.
Diagnostic Procedures
Imaging Techniques
- CT Scan (Computed Tomography): CT scans utilize X-rays to create detailed cross-sectional images of the pancreas and surrounding structures. They are valuable in detecting abnormalities such as tumors, inflammation, or pancreatic cysts.
- MRI (Magnetic Resonance Imaging): MRI uses magnetic fields and radio waves to produce high-resolution images of the pancreas without radiation. MRI is useful for assessing pancreatic tumors, cysts, and abnormalities in pancreatic ducts.
- Ultrasound: Ultrasound imaging uses sound waves to visualize the pancreas and adjacent organs. It is commonly used to detect pancreatic tumors, gallstones, or fluid collections within the abdomen.
Blood Tests
- Pancreatic Enzyme Levels: Blood tests can measure levels of pancreatic enzymes such as amylase and lipase, which may be elevated in cases of pancreatic inflammation or injury.
- Tumor Markers: Certain blood markers, such as CA 19-9, may be elevated in pancreatic cancer, providing additional diagnostic information.
Biopsy
- A biopsy involves obtaining a tissue sample from the pancreas for microscopic examination to confirm the presence of cancer or other abnormalities.
- Biopsies can be obtained through various methods, including endoscopic ultrasound-guided biopsy, fine-needle aspiration, or surgical biopsy.
Treatment Options
Medications
- Pain Management: Pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids, may be prescribed to alleviate abdominal pain associated with pancreatitis or pancreatic cancer.
- Enzyme Replacement Therapy: For individuals with pancreatic insufficiency, enzyme replacement therapy with pancreatic enzyme supplements can aid digestion and alleviate symptoms of malabsorption.
- Insulin Therapy: Individuals with diabetes mellitus may require insulin therapy to regulate blood sugar levels and prevent complications.
Surgery
- Pancreatectomy: Surgical removal of part or all of the pancreas may be necessary for treating pancreatic tumors or severe cases of pancreatitis.
- Whipple Procedure: The Whipple procedure, or pancreaticoduodenectomy, involves removing the head of the pancreas, part of the small intestine, gallbladder, and bile ducts for treating pancreatic cancer located in the head of the pancreas.
- Palliative Surgery: Palliative surgical procedures may be performed to relieve symptoms and improve quality of life in individuals with advanced pancreatic cancer, such as bypass surgery to alleviate obstructive jaundice or placement of stents to relieve bile duct or duodenal obstruction.
Lifestyle Changes
- Dietary Modifications: Adopting a low-fat diet, avoiding alcohol and spicy foods, and consuming small, frequent meals can help manage symptoms of pancreatitis and improve digestive function.
- Smoking Cessation: Quitting smoking is essential for individuals with pancreatic diseases, as smoking is a significant risk factor for pancreatic cancer and can exacerbate pancreatitis.
- Weight Management: Maintaining a healthy weight through diet and exercise is important for preventing obesity-related complications and managing metabolic disorders such as diabetes.
Palliative Care for Advanced Diseases
- Palliative care focuses on relieving symptoms, managing pain, and improving quality of life for individuals with advanced pancreatic diseases.
- Palliative interventions may include pain management, nutritional support, psychosocial support, and coordination of care to address physical, emotional, and spiritual needs.
Prevention and Management
Prevention and management of pancreatic diseases require a comprehensive approach that encompasses lifestyle modifications, regular screenings, and effective disease management strategies. By adopting healthy habits, staying vigilant with check-ups, and adhering to treatment plans, individuals can reduce their risk of developing pancreatic diseases and optimize their overall health and well-being.
Lifestyle Modifications to Reduce the Risk of Pancreatic Diseases
- Healthy Diet: Adopting a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce the risk of pancreatic diseases. Limiting consumption of processed foods, sugary beverages, and saturated fats may also lower the risk.
- Moderate Alcohol Consumption: Limiting alcohol intake to moderate levels can help prevent alcoholic pancreatitis, a leading cause of chronic pancreatitis.
- Maintain a Healthy Weight: Obesity is a risk factor for pancreatic diseases such as pancreatitis and pancreatic cancer. Maintaining a healthy weight through regular exercise and portion control can reduce the risk.
- Avoid Smoking: Smoking is a significant risk factor for pancreatic cancer. Quitting smoking or avoiding tobacco products altogether can help lower the risk of developing pancreatic diseases.
Importance of Regular Check-Ups and Screenings
- Early Detection: Regular check-ups with a healthcare provider can help detect pancreatic diseases early when treatment is most effective. Screening tests such as blood tests, imaging studies, and endoscopic procedures may be recommended for individuals at high risk, such as those with a family history of pancreatic cancer or certain genetic syndromes.
- Monitoring High-Risk Individuals: Individuals with a family history of pancreatic diseases or known risk factors should undergo regular screenings and surveillance to monitor for any signs of disease progression or development.
Strategies for Managing Pancreatic Diseases Effectively
- Adherence to Treatment Plans: Strict adherence to prescribed medications, dietary recommendations, and lifestyle modifications is crucial for managing pancreatic diseases such as pancreatitis and diabetes mellitus.
- Pain Management: Effective pain management strategies, including medications, relaxation techniques, and physical therapy, can help alleviate symptoms and improve quality of life for individuals with chronic pancreatitis or advanced pancreatic cancer.
- Nutritional Support: Nutrition plays a critical role in managing pancreatic diseases, particularly pancreatitis and pancreatic insufficiency. Working with a registered dietitian to develop a tailored nutrition plan can help optimize nutrient intake, prevent malnutrition, and alleviate digestive symptoms.
- Psychosocial Support: Coping with a pancreatic disease can be challenging, both physically and emotionally. Seeking support from family, friends, support groups, or mental health professionals can help individuals navigate the emotional and psychological aspects of their condition.
Conclusion
Early detection, timely intervention, and effective management are key to addressing pancreatic diseases and minimizing their impact on individuals’ health. Lifestyle modifications, regular check-ups, and adherence to treatment plans are essential components of preventive care and disease management strategies.
By adopting healthy habits, staying vigilant with screenings, and seeking appropriate medical care, individuals can reduce their risk of developing pancreatic diseases and optimize their overall health outcomes.