Sepsis, a potentially life-threatening condition, demands immediate attention and understanding. At its core, sepsis occurs when the body’s response to an infection triggers widespread inflammation, leading to organ dysfunction. We delve deep into the nuances of sepsis, exploring its causes, symptoms, diagnosis, treatment, and prevention strategies.
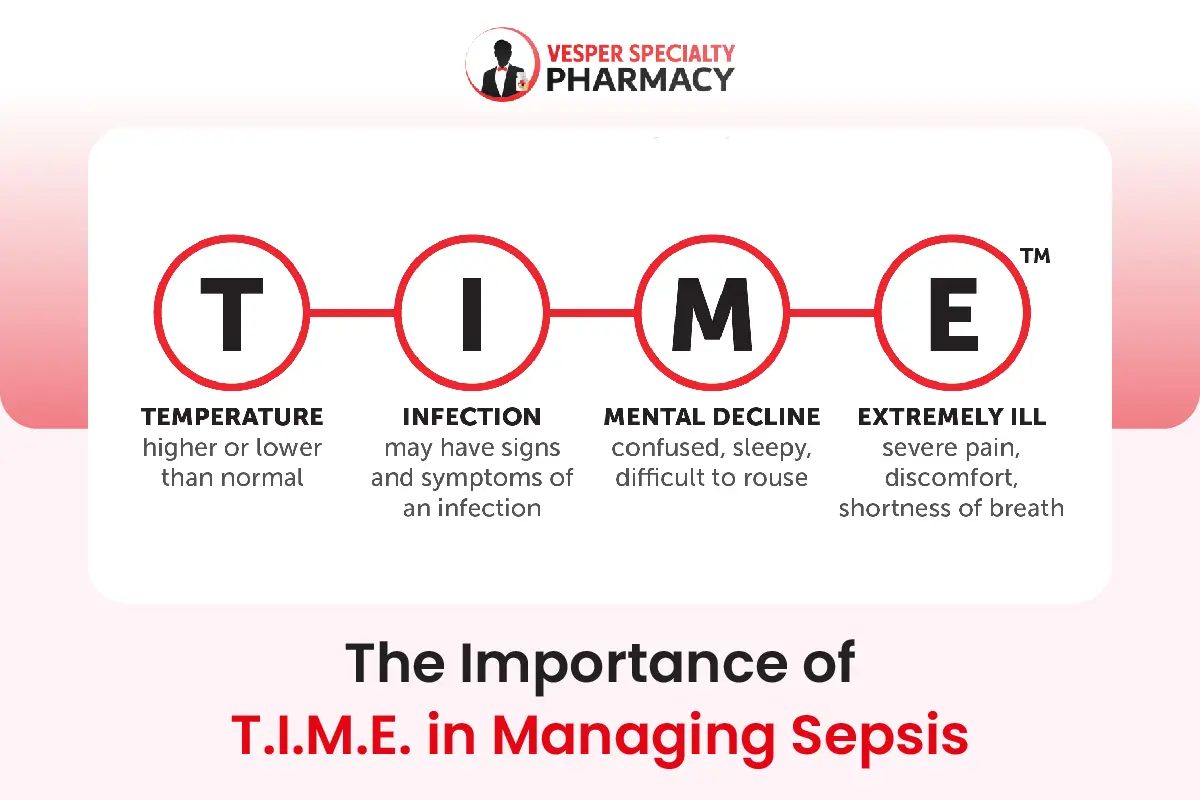
The T.I.M.E. acronym serves as a useful aid in identifying and recalling the indicators of sepsis:
- T: Temperature – Abnormal body temperature, either elevated or lowered.
- I: Infection – Presence of signs and symptoms indicative of an infection.
- M: Mental decline – Altered mental state such as drowsiness, difficulty in awakening, or confusion.
- E: Extremely ill – Exhibiting severe symptoms such as intense pain, discomfort, or difficulty breathing.
Table of Contents
What Causes Sepsis?
Sepsis typically stems from an infection, often bacterial, but can also result from fungal or viral sources. Common infection sites include the lungs, urinary tract, abdomen, and skin. When the body detects an infection, it releases chemicals into the bloodstream to combat it. In some cases, this immune response spirals out of control, leading to sepsis.
Recognizing The Symptoms of Sepsis
Early recognition of sepsis symptoms is crucial for prompt treatment and improved outcomes. Symptoms may include fever, increased heart rate, rapid breathing, altered mental state, and signs of organ dysfunction. Patients may also experience chills, confusion, low blood pressure, and difficulty breathing. Timely intervention significantly enhances the chances of recovery.
Common Signs and Symptoms of Sepsis
Fever or Hypothermia
Sepsis can present with either a high fever or abnormally low body temperature, often accompanied by chills or rigors. Fever may be absent in immunocompromised individuals or those receiving immunosuppressive therapy.
Increased Heart Rate (Tachycardia)
Sepsis-induced systemic inflammation can lead to rapid heart rate, known as tachycardia. Monitoring heart rate is essential for detecting early signs of sepsis and assessing the patient’s hemodynamic status.
Rapid Breathing (Tachypnea)
Respiratory compromise is common in sepsis, resulting in rapid, shallow breathing known as tachypnea. Patients may exhibit increased work of breathing, shortness of breath, or respiratory distress.
Altered Mental Status
Sepsis can affect cognitive function and mental status, leading to confusion, disorientation, or lethargy. Patients may appear agitated, delirious, or unresponsive, indicating impaired cerebral perfusion.
Hypotension
Sepsis-induced vasodilation and fluid loss can cause low blood pressure, known as hypotension. Hypotension may progress to septic shock if left untreated, leading to organ failure and poor prognosis.
Signs of Organ Dysfunction
Sepsis can impair the function of multiple organ systems, resulting in specific clinical manifestations. These may include oliguria (decreased urine output) indicating kidney dysfunction, jaundice suggesting liver involvement, or metabolic acidosis reflecting impaired cellular metabolism.
Red Flags for Sepsis
- SIRS Criteria: The Systemic Inflammatory Response Syndrome (SIRS) criteria, including abnormal body temperature, tachycardia, tachypnea, and abnormal white blood cell count, serve as a screening tool for sepsis. Meeting two or more SIRS criteria in the setting of suspected infection raises suspicion for sepsis.
- Sequential Organ Failure Assessment (SOFA) Score: The SOFA score is a validated tool used to assess the severity of organ dysfunction in critically ill patients, including those with sepsis. Elevated SOFA scores indicate a higher risk of mortality and may prompt further evaluation and intervention.
- Quick Sequential Organ Failure Assessment (qSOFA): The qSOFA score, consisting of altered mental status, systolic hypotension, and tachypnea, helps identify patients at risk of poor outcomes from sepsis outside the intensive care unit (ICU) setting. A qSOFA score of two or more points warrants prompt evaluation for sepsis.
Clinical Evaluation and Diagnosis
Diagnosing sepsis involves a comprehensive assessment of clinical symptoms, laboratory findings, and imaging studies. Healthcare providers should maintain a high index of suspicion for sepsis in patients with suspected or confirmed infections, especially in those with predisposing factors such as immunosuppression, advanced age, or chronic medical conditions. Prompt recognition and early initiation of appropriate treatment are crucial for optimizing patient outcomes and reducing the morbidity and mortality associated with sepsis.
Diagnostic Approaches
Diagnosing sepsis involves a comprehensive evaluation of clinical symptoms, laboratory tests, and imaging studies. Blood cultures help identify the causative organism, while other tests assess organ function and the severity of infection. Imaging modalities such as X-rays and CT scans aid in detecting potential sources of infection and complications.
Treatment Strategies
Immediate treatment of sepsis revolves around aggressive antibiotic therapy to target the underlying infection. Intravenous fluids are administered to maintain adequate blood pressure and organ perfusion. In severe cases, vasopressor medications may be necessary to stabilize blood pressure. Intensive care support, including mechanical ventilation and kidney dialysis, may be required for organ support.
Antibiotic Therapy
Prompt administration of broad-spectrum antibiotics is a cornerstone of sepsis treatment. Empirical antibiotic therapy should be initiated as soon as sepsis is suspected, without waiting for definitive culture results.
The choice of antibiotics should be guided by local antimicrobial resistance patterns and the suspected source of infection. Antibiotic therapy may be adjusted based on culture results and the patient’s response to treatment.
Intravenous Fluids
Intravenous fluid resuscitation is essential for maintaining adequate tissue perfusion and hemodynamic stability in patients with sepsis-induced hypotension or shock. Crystalloid solutions, such as normal saline or balanced electrolyte solutions, are commonly used for fluid resuscitation. The goal is to restore intravascular volume and optimize cardiac output while monitoring for signs of fluid overload.
Vasopressor Therapy
In patients with refractory hypotension despite fluid resuscitation, vasopressor medications may be necessary to maintain adequate blood pressure and organ perfusion. Vasopressors, such as norepinephrine or dopamine, work by constricting blood vessels and increasing systemic vascular resistance. Careful titration of vasopressor therapy is crucial to avoid adverse effects such as tissue ischemia and arrhythmias.
Supportive Care
Supportive care measures are essential in managing sepsis-related complications and organ dysfunction. Mechanical ventilation may be required for patients with respiratory failure, while renal replacement therapy may be necessary for those with acute kidney injury. Close monitoring of vital signs, fluid balance, and laboratory parameters is critical for early detection of complications and timely intervention.
Source Control
Identifying and addressing the source of infection is paramount in sepsis management. This may involve surgical intervention, such as drainage of abscesses or debridement of infected tissues, to remove the source of infection and prevent its spread. Timely source control measures help reduce the bacterial burden and improve the effectiveness of antibiotic therapy.
Adjunctive Therapies
Several adjunctive therapies have been investigated for the treatment of sepsis, although their efficacy remains controversial. These may include corticosteroids, intravenous immunoglobulins, and activated protein C. The use of these adjunctive therapies should be individualized based on the patient’s clinical presentation, underlying comorbidities, and response to standard treatment measures.
Multidisciplinary Approach
Sepsis management requires a multidisciplinary approach involving collaboration among healthcare professionals from various specialties, including critical care, infectious diseases, pharmacy, nursing, and respiratory therapy. Effective communication, coordination of care, and adherence to evidence-based guidelines are essential for optimizing patient outcomes.
Preventing Sepsis
Prevention lies at the forefront of combating sepsis. Simple measures such as hand hygiene, proper wound care, and vaccination against preventable infections can significantly reduce the risk of sepsis.
Early recognition and treatment of infections, particularly in vulnerable populations such as the elderly and those with weakened immune systems, are paramount in preventing sepsis-related complications.
Hand Hygiene
Hand hygiene is the cornerstone of infection prevention. Proper handwashing with soap and water, or the use of alcohol-based hand sanitizers, can effectively eliminate harmful bacteria and viruses. Encouraging regular hand hygiene practices among healthcare professionals, patients, and the general public is crucial in preventing the spread of infections that can lead to sepsis.
Wound Care
Prompt and proper wound care is essential in preventing infections that can progress to sepsis. Cleaning wounds thoroughly with mild soap and water, applying appropriate dressings, and seeking medical attention for signs of infection are vital steps in wound management. Timely intervention can prevent the spread of infection and reduce the risk of sepsis-related complications.
Vaccination
Vaccination plays a pivotal role in preventing infections that are common culprits in sepsis development. Immunizations against influenza, pneumonia, meningitis, and other vaccine-preventable diseases not only protect individuals from contracting these infections but also contribute to community-wide immunity. By reducing the prevalence of infectious diseases, vaccination helps curb the incidence of sepsis and its associated morbidity and mortality.
Infection Control Practices
In healthcare settings, strict adherence to infection control practices is imperative in preventing healthcare-associated infections (HAIs) that can lead to sepsis. Measures such as proper sterilization of medical equipment, adherence to aseptic techniques during procedures, and isolation precautions for patients with contagious infections help minimize the spread of pathogens. Comprehensive infection control protocols, coupled with ongoing staff education and training, are essential components of a robust strategy to prevent sepsis in healthcare facilities.
Early Recognition and Treatment of Infections
Timely recognition and treatment of infections are pivotal in preventing their progression to sepsis. Healthcare providers must remain vigilant for signs and symptoms of infection, particularly in high-risk populations such as the elderly, individuals with compromised immune systems, and those with chronic medical conditions. Prompt initiation of appropriate antimicrobial therapy, coupled with supportive care measures, can halt the advancement of infection and prevent the onset of sepsis.
Patient Education
Empowering patients and their caregivers with knowledge about sepsis risk factors, signs, and preventive measures is essential in reducing the incidence of this condition. Educational initiatives aimed at raising awareness about hand hygiene, wound care, vaccination, and infection control practices can empower individuals to take proactive steps in safeguarding their health. By fostering a culture of prevention and self-care, healthcare providers can play a pivotal role in preventing sepsis and promoting overall wellness in their communities.
Conclusion
Sepsis remains a formidable challenge in modern healthcare, requiring a multidisciplinary approach for optimal management. By understanding its causes, recognizing early symptoms, implementing timely interventions, and prioritizing prevention strategies, we can effectively combat sepsis and improve patient outcomes. Stay informed, stay vigilant, and together, we can mitigate the impact of this potentially deadly condition.