Type 1 Diabetes, often referred to as juvenile diabetes or insulin-dependent diabetes, is a chronic autoimmune condition characterized by the body’s inability to produce insulin. Unlike Type 2 Diabetes, which is primarily influenced by lifestyle factors, Type 1 Diabetes typically develops early in life, although it can occur at any age.
Table of Contents
What Is Type 1 Diabetes?
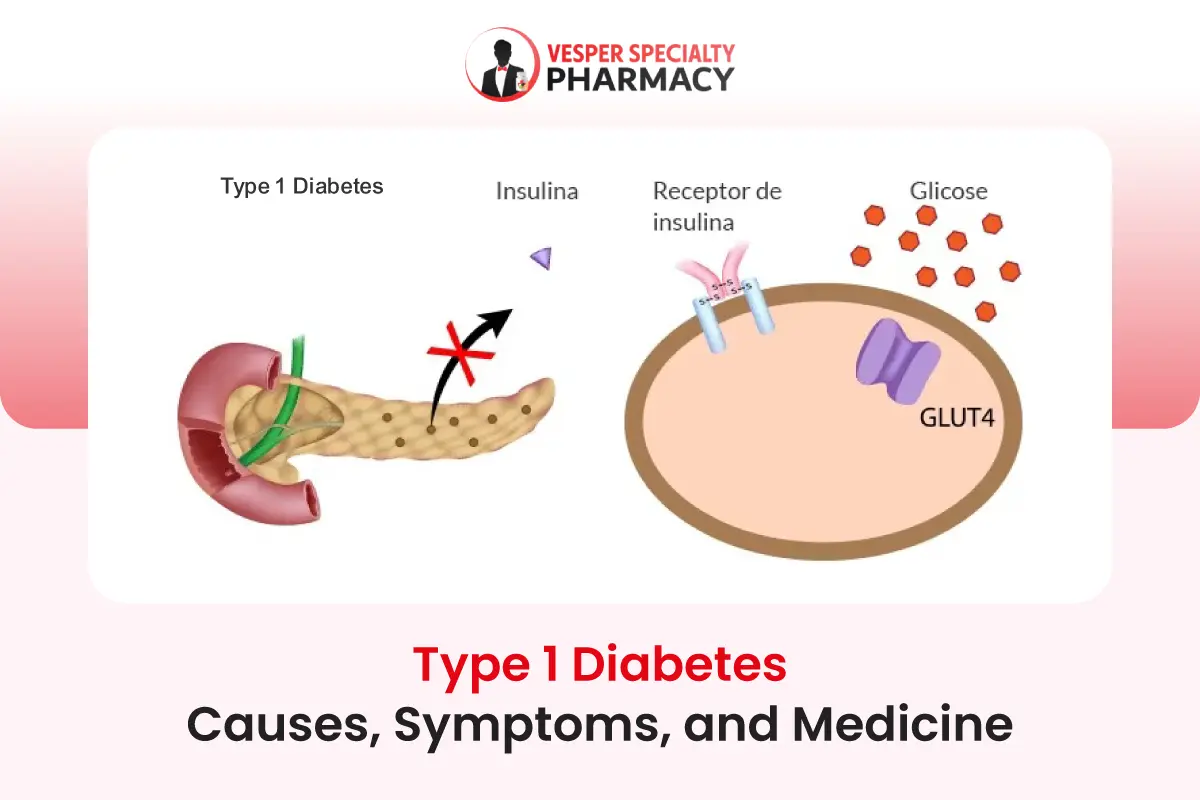
Type 1 Diabetes occurs when the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. Insulin is a hormone that regulates blood sugar levels by facilitating the uptake of glucose into cells for energy. Without sufficient insulin, glucose accumulates in the bloodstream, leading to high blood sugar levels (hyperglycemia), which can cause various complications if left unmanaged.
Importance of Understanding The Condition
Understanding Type 1 Diabetes is crucial for several reasons. Firstly, it affects approximately 10% of people with diabetes worldwide, making it a significant health concern. Secondly, unlike Type 2 Diabetes, which can sometimes be managed through lifestyle changes, Type 1 Diabetes requires lifelong insulin therapy for survival. Thirdly, proper management of Type 1 Diabetes is essential to prevent complications such as cardiovascular disease, kidney failure, and vision problems.
Furthermore, awareness of Type 1 Diabetes is vital for early detection and prompt treatment. Recognizing the symptoms and seeking medical attention promptly can help individuals with Type 1 Diabetes lead healthier lives and reduce the risk of long-term complications.
Additionally, understanding the condition fosters empathy and support for those living with Type 1 Diabetes, promoting inclusivity and understanding within communities.
Genetics and Environmental Factors Contributing to its Development
Genetics play a significant role in the susceptibility to Type 1 Diabetes, although the exact genes involved are complex and not fully understood. Individuals with a family history of Type 1 Diabetes have a higher risk of developing the condition. However, genetics alone cannot account for the rising incidence of Type 1 Diabetes, suggesting the involvement of environmental factors as well.
Various environmental triggers have been implicated in the development of Type 1 Diabetes, including viral infections, dietary factors, and exposure to certain toxins. Viral infections, particularly during childhood, can trigger an autoimmune response that targets the beta cells in susceptible individuals.
Additionally, dietary factors, such as early introduction of cow’s milk or gluten-containing foods, have been associated with an increased risk of developing Type 1 Diabetes in some studies.
Autoimmune Nature of the Disease
In Type 1 Diabetes, the body’s immune system mistakenly identifies the beta cells in the pancreas as foreign invaders and launches an attack against them. This autoimmune response leads to inflammation and destruction of the beta cells, resulting in a significant reduction or complete cessation of insulin production. Without insulin, glucose cannot enter cells effectively, causing it to accumulate in the bloodstream, leading to hyperglycemia.
Difference Between Type 1 Diabetes and Type 2 Diabetes
While both Type 1 and Type 2 Diabetes involve issues with insulin regulation and blood sugar control, they have distinct underlying mechanisms and risk factors. Type 1 Diabetes is primarily an autoimmune disease that often develops in childhood or adolescence, although it can occur at any age. It requires lifelong insulin therapy for management.
On the other hand, Type 2 Diabetes typically develops later in life and is associated with insulin resistance, where the body’s cells become less responsive to insulin. This leads to compensatory insulin production by the pancreas, but over time, the pancreas may not be able to keep up with the demand, resulting in relative insulin deficiency. Type 2 Diabetes is often managed with lifestyle modifications, oral medications, and sometimes insulin therapy.
Causes of Type 1 Diabetes
Type 1 Diabetes is a complex condition influenced by both genetic and environmental factors. Understanding the underlying causes is essential for elucidating the disease’s pathogenesis and developing effective preventive and therapeutic strategies. Here are the key factors contributing to the development of Type 1 Diabetes:
Genetic Predisposition and Family History
Genetics play a significant role in the susceptibility to Type 1 Diabetes. Individuals with certain genetic markers, particularly those related to the human leukocyte antigen (HLA) complex, have an increased risk of developing the condition. HLA genes are involved in the regulation of the immune system, and specific variants are associated with an elevated risk of autoimmune diseases, including Type 1 Diabetes.
Moreover, having a family history of Type 1 Diabetes further increases the likelihood of developing the condition. Relatives of individuals with Type 1 Diabetes have a higher risk compared to the general population, indicating a strong genetic component in disease predisposition.
Autoimmune Response Targeting Insulin-Producing Cells
Type 1 Diabetes is fundamentally an autoimmune disease characterized by the immune system’s misguided attack on the insulin-producing beta cells in the pancreas. Normally, the immune system functions to protect the body against foreign invaders, such as bacteria and viruses. However, in individuals with Type 1 Diabetes, the immune system mistakenly identifies beta cells as threats and mounts an immune response against them.
This autoimmune attack leads to inflammation and destruction of the beta cells, impairing their ability to produce insulin. As a result, insulin deficiency develops, leading to dysregulation of blood sugar levels and the characteristic symptoms of Type 1 Diabetes.
Potential Triggers Such as Viral Infections
While genetic predisposition lays the groundwork for the development of Type 1 Diabetes, environmental factors are believed to trigger the autoimmune response in susceptible individuals.
One such trigger is viral infections, particularly during childhood. Viruses such as enteroviruses, coxsackievirus, and rubella have been implicated in initiating or accelerating the autoimmune process in genetically predisposed individuals.
These viruses may provoke an immune response that not only targets the virus itself but also inadvertently attacks beta cells in the pancreas. Additionally, certain viral infections can cause inflammation and damage to pancreatic tissue, further contributing to the development of Type 1 Diabetes.
Overall, the interplay between genetic susceptibility and environmental triggers plays a crucial role in the pathogenesis of Type 1 Diabetes. Identifying these factors is essential for understanding disease development and progression, as well as for developing targeted interventions aimed at preventing or delaying the onset of Type 1 Diabetes in at-risk individuals.
Symptoms of Type 1 Diabetes
It’s important to note that while these symptoms are common in Type 1 Diabetes, they can also be indicative of other health conditions. If you or someone you know experiences any of these symptoms, especially in combination, it’s essential to seek medical attention for proper evaluation and diagnosis.
Recognizing the symptoms of Type 1 Diabetes is crucial for early detection and prompt treatment. The condition can manifest with various signs and symptoms, which may develop rapidly over a short period. Early detection and management of Type 1 Diabetes are crucial for preventing complications and improving long-term health outcomes. Here are the common symptoms of Type 1 Diabetes:
Excessive Thirst and Urination
One of the hallmark symptoms of Type 1 Diabetes is polyuria or excessive urination. This occurs as a result of elevated blood sugar levels, which spill into the urine and draw water from the body’s tissues.
As a result, individuals with Type 1 Diabetes may experience frequent urination, especially during the night (nocturia). Excessive urination can lead to dehydration, triggering increased thirst (polydipsia) as the body attempts to replenish lost fluids.
Sudden Weight Loss
Unexplained weight loss is another common symptom of Type 1 Diabetes, particularly in the early stages of the disease.
Despite increased hunger and food intake, individuals with Type 1 Diabetes may experience unintentional weight loss due to the body’s inability to utilize glucose for energy.
In the absence of sufficient insulin, the body begins to break down stored fat and muscle tissue for energy, leading to weight loss.
Fatigue and Weakness
Persistent fatigue and weakness are often reported by individuals with Type 1 Diabetes. The lack of insulin prevents glucose from entering cells to be used as fuel, resulting in energy depletion and feelings of fatigue.
Additionally, the breakdown of fats and proteins for energy in the absence of glucose further contributes to feelings of weakness and lethargy.
Increased Hunger
Despite experiencing weight loss, individuals with Type 1 Diabetes may also experience increased hunger (polyphagia).
This occurs as a result of the body’s inability to utilize glucose properly, leading to cellular starvation despite high levels of circulating glucose in the bloodstream.
The brain perceives this as hunger and signals for increased food intake, even though the body is unable to properly metabolize glucose for energy.
Blurred Vision
Changes in vision, such as blurred vision or fluctuations in eyesight, can occur in individuals with Type 1 Diabetes. Elevated blood sugar levels can lead to swelling of the lens in the eye, causing temporary changes in vision.
Additionally, uncontrolled diabetes can increase the risk of developing long-term eye complications, such as diabetic retinopathy, which can lead to permanent vision loss if left untreated.
How To Diagnosis Type 1 Diabetes?
Accurate diagnosis of Type 1 Diabetes is essential for initiating appropriate treatment and preventing complications. Healthcare providers use various tests to confirm the presence of the condition and assess its severity. Here are the key diagnostic tests for Type 1 Diabetes:
1. Blood Tests Measuring Blood Sugar Levels
Blood tests measuring blood sugar levels, specifically fasting plasma glucose (FPG) and random plasma glucose (RPG) tests, are commonly used to diagnose diabetes. In individuals suspected of having Type 1 Diabetes, blood glucose levels are typically significantly elevated due to insulin deficiency.
A fasting plasma glucose test measures blood sugar levels after an overnight fast, while a random plasma glucose test can be performed at any time of the day. Elevated blood glucose levels above established thresholds indicate diabetes.
2. Glycated Hemoglobin (A1C) Test
The glycated hemoglobin (A1C) test provides information about average blood sugar levels over the past two to three months. It measures the percentage of hemoglobin that is glycated (bound to glucose) in the bloodstream. For individuals with Type 1 Diabetes, A1C levels are typically elevated due to persistently high blood sugar levels. An A1C level of 6.5% or higher is indicative of diabetes.
The A1C test is particularly useful for monitoring long-term blood sugar control and assessing the effectiveness of diabetes management strategies. It provides valuable information for healthcare providers to adjust treatment regimens and prevent complications associated with poorly controlled diabetes.
3. C-Peptide Test to Determine Insulin Production
The C-peptide test measures the level of C-peptide, a protein that is released along with insulin when the pancreas produces insulin. Since insulin is produced in insufficient quantities or not at all in individuals with Type 1 Diabetes, C-peptide levels are typically low in these individuals.
Measuring C-peptide levels helps differentiate between Type 1 and Type 2 Diabetes, as individuals with Type 2 Diabetes often have normal or elevated C-peptide levels due to insulin resistance.
Low C-peptide levels, in conjunction with other diagnostic criteria such as elevated blood glucose levels and symptoms of diabetes, support the diagnosis of Type 1 Diabetes. This test aids healthcare providers in determining the appropriate treatment approach and assessing the need for insulin therapy.
Effective Management of Type 1 Diabetes
Effective management of Type 1 Diabetes is essential for maintaining blood sugar levels within target ranges, preventing complications, and promoting overall well-being.
A comprehensive approach to Type 1 Diabetes management, including insulin therapy, blood sugar monitoring, healthy eating, and regular exercise, empowers individuals to achieve optimal blood sugar control, minimize complications, and lead fulfilling lives despite their condition. Here’s an overview of each component of Type 1 Diabetes management:
1. Insulin Therapy: Different Types of Insulin and Administration Methods
Insulin therapy is the cornerstone of Type 1 Diabetes management, as individuals with the condition require exogenous insulin to replace the insulin their bodies cannot produce. Several types of insulin are available, categorized based on their onset, peak, and duration of action:
- Rapid-acting Insulin: Begins to work within minutes and peaks within 1-2 hours after injection. Examples include insulin aspart, insulin lispro, and insulin glulisine.
- Short-acting Insulin: Starts working within 30 minutes to 1 hour and peaks within 2-3 hours after injection. Regular human insulin is an example of short-acting insulin.
- Intermediate-acting Insulin: Begins to work within 1-2 hours and peaks within 4-12 hours after injection. NPH insulin is a commonly used intermediate-acting insulin.
- Long-acting Insulin: Provides a steady level of insulin over a longer duration, typically lasting up to 24 hours. Examples include insulin glargine and insulin detemir.
Insulin can be administered via injection using insulin syringes, insulin pens, or insulin pumps. Continuous subcutaneous insulin infusion (CSII) through insulin pumps offers flexibility in insulin delivery and mimics the body’s natural insulin secretion pattern more closely.
2. Blood Sugar Monitoring: Importance and Techniques
Regular blood sugar monitoring is crucial for individuals with Type 1 Diabetes to assess their blood glucose levels and adjust insulin doses accordingly. Continuous glucose monitoring (CGM) systems provide real-time glucose readings throughout the day, offering insights into blood sugar patterns and trends.
Additionally, self-monitoring of blood glucose (SMBG) using glucometers allows individuals to check their blood sugar levels at various times, such as before meals, after meals, before exercise, and at bedtime. These measurements help individuals make informed decisions about insulin dosing, dietary choices, and physical activity levels.
3. Healthy Eating: Balancing Carbohydrates, Proteins, and Fats
A balanced diet plays a vital role in managing blood sugar levels in individuals with Type 1 Diabetes. Carbohydrates have the most significant impact on blood sugar levels, so monitoring carbohydrate intake and distributing it evenly throughout the day is essential. Meals should include a combination of carbohydrates, proteins, and fats to promote satiety and provide sustained energy.
Carbohydrate counting is a common dietary approach used by individuals with Type 1 Diabetes to estimate the amount of insulin needed to cover carbohydrate intake. This involves calculating the carbohydrate content of foods and matching it with insulin doses to maintain blood sugar control.
4. Regular Exercise: Benefits and Precautions
Regular physical activity offers numerous benefits for individuals with Type 1 Diabetes, including improved insulin sensitivity, better blood sugar control, and reduced risk of cardiovascular complications. Exercise helps lower blood sugar levels by increasing glucose uptake into muscles for energy and enhancing insulin action.
However, individuals with Type 1 Diabetes should take precautions when exercising to prevent hypoglycemia (low blood sugar). It’s essential to monitor blood sugar levels before, during, and after exercise and adjust insulin doses or carbohydrate intake as needed.
Additionally, staying hydrated and carrying fast-acting carbohydrates, such as glucose tablets or fruit juice, can help manage blood sugar levels during physical activity.
Complications of Type 1 Diabetes
Type 1 Diabetes, when left uncontrolled, can lead to various short-term and long-term complications that significantly impact overall health and quality of life.
Proper management of Type 1 Diabetes, including maintaining blood sugar levels within target ranges, adopting a healthy lifestyle, and undergoing regular medical screenings, is essential for reducing the risk of complications and promoting long-term health and well-being.
It’s essential for individuals with Type 1 Diabetes to be aware of these complications and take proactive steps to manage their condition effectively. Here’s an overview of the potential complications:
Short-Term Complications
Short-term complications of Type 1 Diabetes can occur suddenly and require immediate intervention to prevent serious health consequences:
Hypoglycemia (Low Blood Sugar)
Hypoglycemia occurs when blood sugar levels drop below normal levels (typically below 70 mg/dL). It can result from excessive insulin dosage, delayed or missed meals, increased physical activity, or alcohol consumption.
Symptoms of hypoglycemia include shakiness, sweating, dizziness, confusion, and rapid heartbeat. If left untreated, severe hypoglycemia can lead to loss of consciousness, seizures, and even death.
Hyperglycemia (High Blood Sugar)
Hyperglycemia refers to persistently high blood sugar levels, usually above the target range (typically above 180 mg/dL). It can result from insufficient insulin dosage, overeating, illness, stress, or lack of physical activity.
Symptoms of hyperglycemia include increased thirst, frequent urination, fatigue, blurred vision, and slow wound healing.
If left untreated, severe hyperglycemia can lead to diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS), both of which are life-threatening conditions requiring immediate medical attention.
Long-Term Complications
Long-term complications of Type 1 Diabetes develop gradually over time and can affect various organs and systems in the body:
Cardiovascular Diseases
Individuals with Type 1 Diabetes have an increased risk of developing cardiovascular diseases, including coronary artery disease, heart attack, and stroke. Chronic high blood sugar levels can damage blood vessels and nerves, leading to atherosclerosis (hardening and narrowing of arteries) and increased risk of cardiovascular events.
Nerve Damage (Neuropathy)
Diabetic neuropathy is a common complication of Type 1 Diabetes that affects the nerves, particularly those in the legs and feet. Symptoms may include numbness, tingling, burning sensations, or pain in the affected areas. Neuropathy can lead to complications such as diabetic foot ulcers, infections, and even limb amputation if left untreated.
Kidney Damage (Nephropathy)
Diabetic nephropathy is a type of kidney damage that occurs as a result of prolonged high blood sugar levels. It can lead to impaired kidney function, proteinuria (excess protein in the urine), and eventually kidney failure if left untreated.
Early detection and management of diabetic nephropathy are crucial to prevent or delay progression to end-stage renal disease (ESRD) requiring dialysis or kidney transplantation.
Eye Problems (Retinopathy)
Diabetic retinopathy is a leading cause of vision loss and blindness among individuals with Type 1 Diabetes. Prolonged high blood sugar levels can damage the blood vessels in the retina, leading to diabetic retinopathy.
Symptoms may include blurred vision, floaters, or difficulty seeing at night. Regular eye examinations and early intervention are essential to prevent vision loss and preserve eye health.
Recommended Medicines for Type 1 Diabetes in Las Vegas
In Las Vegas, individuals with Type 1 Diabetes have access to a variety of medications to help manage their condition effectively. These medications aim to regulate blood sugar levels, improve insulin sensitivity, and prevent complications associated with diabetes.
The selection of medications for Type 1 Diabetes management in Las Vegas should be individualized based on factors such as blood sugar control, lifestyle preferences, and the presence of comorbidities.
Healthcare providers work closely with patients to develop personalized treatment plans that optimize blood sugar control and minimize the risk of complications associated with diabetes.
Here are the recommended examples of medicines for Type 1 Diabetes in Las Vegas:
1. Insulin Analogs: Types Available and Their Mechanisms of Action
Insulin analogs are synthetic forms of insulin that mimic the body’s natural insulin secretion more closely, providing more predictable and consistent blood sugar control compared to traditional insulin formulations. There are several types of insulin analogs available, each with its onset, peak, and duration of action:
Rapid-Acting Insulin Analogs
These insulins, such as insulin aspart (NovoLog), insulin lispro (Humalog), and insulin glulisine (Apidra), have a rapid onset of action (within 15 minutes) and peak within 1-2 hours after injection. They are typically administered before meals to control postprandial blood sugar spikes.
Short-Acting Insulin Analogs
Short-acting insulins, such as regular insulin, have a slightly slower onset of action (within 30 minutes to 1 hour) and peak within 2-3 hours after injection. They are commonly used to cover meals and snacks.
Intermediate-Acting Insulin Analogs
Intermediate-acting insulins, such as NPH insulin, have a delayed onset of action (1-2 hours) and peak within 4-12 hours after injection. They provide basal insulin coverage and may be used in combination with rapid-acting or short-acting insulins.
Long-Acting Insulin Analogs
Long-acting insulins, such as insulin glargine (Lantus, Basaglar) and insulin detemir (Levemir), provide a steady level of insulin over an extended period (up to 24 hours). They are typically administered once daily to provide basal insulin coverage throughout the day and night.
2. Injectable Medications: GLP-1 Receptor Agonists and Amylin Analogs
In addition to insulin therapy, certain injectable medications may be used as adjunct therapies to improve blood sugar control in individuals with Type 1 Diabetes:
GLP-1 Receptor Agonists
Glucagon-like peptide-1 (GLP-1) receptor agonists, such as liraglutide (Victoza) and exenatide (Byetta, Bydureon), stimulate insulin secretion, inhibit glucagon release, and delay gastric emptying, resulting in lower blood sugar levels. They may be used in combination with insulin therapy to reduce insulin doses and aid in weight management.
Amylin Analogs
Amylin is a hormone co-secreted with insulin by the pancreas. Synthetic amylin analogs, such as pramlintide (Symlin), mimic the effects of natural amylin, including slowing gastric emptying, suppressing glucagon secretion, and promoting satiety. They are used as adjunct therapies to insulin to improve postprandial blood sugar control and reduce the risk of hypoglycemia.
3. Oral Medications: Adjunct Therapies for Managing Blood Sugar Levels
While oral medications are not typically used as first-line treatments for Type 1 Diabetes, they may be prescribed as adjunct therapies in certain cases:
SGLT2 Inhibitors
Sodium-glucose cotransporter-2 (SGLT2) inhibitors, such as empagliflozin (Jardiance) and dapagliflozin (Farxiga), work by inhibiting glucose reabsorption in the kidneys, leading to increased urinary glucose excretion and lower blood sugar levels.
They are primarily used in individuals with Type 1 Diabetes who have difficulty achieving glycemic control with insulin therapy alone.
DPP-4 Inhibitors
Dipeptidyl peptidase-4 (DPP-4) inhibitors, such as sitagliptin (Januvia) and saxagliptin (Onglyza), enhance insulin secretion and suppress glucagon release in response to elevated blood sugar levels.
They may be used as adjunct therapies to insulin to improve glycemic control, particularly in individuals with Type 1 Diabetes who are overweight or obese.
Lifestyle Modifications
Adopting a healthy lifestyle is essential for effectively managing Type 1 Diabetes and minimizing the risk of complications. Lifestyle modifications play a crucial role in achieving optimal blood sugar control, enhancing overall well-being, and improving long-term health outcomes. Here’s a closer look at the importance of lifestyle modifications for individuals with Type 1 Diabetes:
Importance of a Healthy Lifestyle in Managing Type 1 Diabetes
Maintaining a healthy lifestyle is paramount for individuals with Type 1 Diabetes to achieve and maintain optimal blood sugar levels. A balanced diet, regular physical activity, stress management, adequate sleep, and avoidance of harmful habits such as smoking are key components of a healthy lifestyle.
These lifestyle factors not only help regulate blood sugar levels but also reduce the risk of cardiovascular disease, nerve damage, kidney damage, and other complications associated with diabetes.
A healthy lifestyle also supports overall well-being and quality of life, allowing individuals with Type 1 Diabetes to lead active, fulfilling lives despite their condition. By prioritizing healthy lifestyle habits, individuals can better manage their diabetes, reduce the need for medication, and minimize the risk of long-term complications.
Incorporating Regular Physical Activity
Regular physical activity offers numerous benefits for individuals with Type 1 Diabetes, including improved insulin sensitivity, better blood sugar control, weight management, and reduced risk of cardiovascular complications. Exercise helps lower blood sugar levels by increasing glucose uptake into muscles for energy and enhancing insulin action.
Incorporating a variety of aerobic exercises, such as walking, jogging, cycling, swimming, and dancing, as well as strength training exercises, can help individuals with Type 1 Diabetes improve their overall fitness levels and manage their condition more effectively.
It’s important to engage in physical activity regularly, aiming for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, as recommended by health authorities.
Monitoring Blood Sugar Levels and Adhering to Medication Regimens
Regular monitoring of blood sugar levels is essential for individuals with Type 1 Diabetes to assess their glycemic control and make informed decisions about insulin dosing, dietary choices, and physical activity levels. Blood sugar monitoring allows individuals to identify patterns and trends in their blood sugar levels and adjust their treatment regimens accordingly.
In addition to blood sugar monitoring, adhering to medication regimens prescribed by healthcare providers is crucial for managing Type 1 Diabetes effectively. This includes taking insulin as prescribed, following dosing instructions, and maintaining a consistent schedule for medication administration. Skipping doses or deviating from prescribed treatment regimens can lead to fluctuations in blood sugar levels and increase the risk of complications.
By monitoring blood sugar levels regularly and adhering to medication regimens, individuals with Type 1 Diabetes can maintain stable blood sugar control, reduce the risk of hypoglycemia and hyperglycemia, and improve overall health and well-being. These lifestyle modifications, combined with other aspects of diabetes management, form the foundation for successful Type 1 Diabetes management and promote better long-term outcomes.
Support Resources for Type 1 Diabetes in Las Vegas
Living with Type 1 Diabetes can present various challenges, but individuals in Las Vegas have access to a range of support resources to help them navigate their diabetes journey effectively. These resources provide education, emotional support, and access to specialized healthcare professionals. Here are some valuable support resources available for individuals with Type 1 Diabetes in Las Vegas:
Diabetes Education Programs
Diabetes education programs offer valuable resources and support to individuals with Type 1 Diabetes, helping them learn about their condition, develop self-management skills, and make informed decisions about their health. These programs typically cover topics such as blood sugar monitoring, insulin administration, healthy eating, physical activity, medication management, and coping strategies.
In Las Vegas, individuals with Type 1 Diabetes can enroll in diabetes education programs offered by local healthcare facilities, community centers, and nonprofit organizations. These programs may include individualized counseling sessions, group classes, workshops, and educational materials to empower individuals to take control of their diabetes and improve their quality of life.
Support Groups and Online Communities
Support groups and online communities provide a valuable source of emotional support, encouragement, and shared experiences for individuals living with Type 1 Diabetes. These groups offer a safe and supportive environment where individuals can connect with others who understand what they’re going through, share tips and strategies for managing diabetes, and exchange information about resources and treatment options.
In Las Vegas, there are various support groups for individuals with Type 1 Diabetes, including local meetups, peer-led support groups, and online communities on social media platforms and diabetes-related websites. These groups provide opportunities for individuals to connect, share stories, ask questions, and seek advice from others who are facing similar challenges.
Access to Specialized Healthcare Professionals
Access to specialized healthcare professionals, such as endocrinologists, diabetes educators, dietitians, and mental health professionals, is essential for comprehensive Type 1 Diabetes management. These healthcare professionals have expertise in managing diabetes and can provide personalized care, guidance, and support to individuals with Type 1 Diabetes.
In Las Vegas, individuals with Type 1 Diabetes can access specialized healthcare professionals through local hospitals, clinics, and private practices specializing in diabetes care. These professionals work collaboratively with patients to develop personalized treatment plans, address individual needs and preferences, and optimize diabetes management strategies to achieve optimal health outcomes.
Overall, the support resources available for individuals with Type 1 Diabetes in Las Vegas play a crucial role in empowering them to live well with their condition. By accessing education programs, support groups, and specialized healthcare professionals, individuals can enhance their diabetes management skills, improve their quality of life, and thrive despite the challenges of living with Type 1 Diabetes.
Conclusion
Type 1 Diabetes is a chronic autoimmune condition characterized by insulin deficiency, requiring lifelong management to maintain optimal health and well-being. Throughout this discussion, we’ve highlighted several key points about Type 1 Diabetes and emphasized the importance of early detection, proper management, and support for individuals living with the condition.
Type 1 Diabetes differs from Type 2 Diabetes in its autoimmune nature, genetic predisposition, and reliance on insulin therapy for management. It’s essential for individuals with Type 1 Diabetes to understand the causes, symptoms, and potential complications of the condition to facilitate early detection and intervention.
While living with Type 1 Diabetes presents challenges, individuals with the condition need to remain proactive, resilient, and optimistic. With proper management, support, and determination, individuals with Type 1 Diabetes can lead fulfilling lives, pursue their goals and aspirations, and thrive despite the challenges posed by their condition.
By staying informed, proactive, and connected to supportive communities, individuals with Type 1 Diabetes can overcome obstacles, achieve their full potential, and embrace life to the fullest.