Type 2 diabetes is a chronic metabolic disorder characterized by high blood sugar levels, insulin resistance, and relative insulin deficiency. Unlike type 1 diabetes, where the body fails to produce insulin altogether, type 2 diabetes typically develops over time and is closely linked to lifestyle factors and genetic predisposition.
Overview of Type 2 Diabetes
Type 2 diabetes accounts for the majority of diabetes cases worldwide, representing around 90-95% of all diagnoses. It often develops in adults, though it’s increasingly diagnosed in children and adolescents due to rising obesity rates. In this condition, the body either becomes resistant to the effects of insulin or doesn’t produce enough insulin to maintain normal blood sugar levels.
Importance of Understanding the Condition
Understanding type 2 diabetes is crucial due to its prevalence and significant impact on health. If left untreated or poorly managed, it can lead to serious complications such as heart disease, stroke, kidney failure, blindness, and nerve damage. However, with proper knowledge and management, individuals with type 2 diabetes can lead healthy and fulfilling lives.
Purpose of the Blog Post
The purpose of this blog post is to provide a comprehensive overview of type 2 diabetes, including its causes, symptoms, and management strategies. By increasing awareness and understanding of this condition, readers can better recognize its signs, take proactive measures for prevention, and effectively manage it if diagnosed.
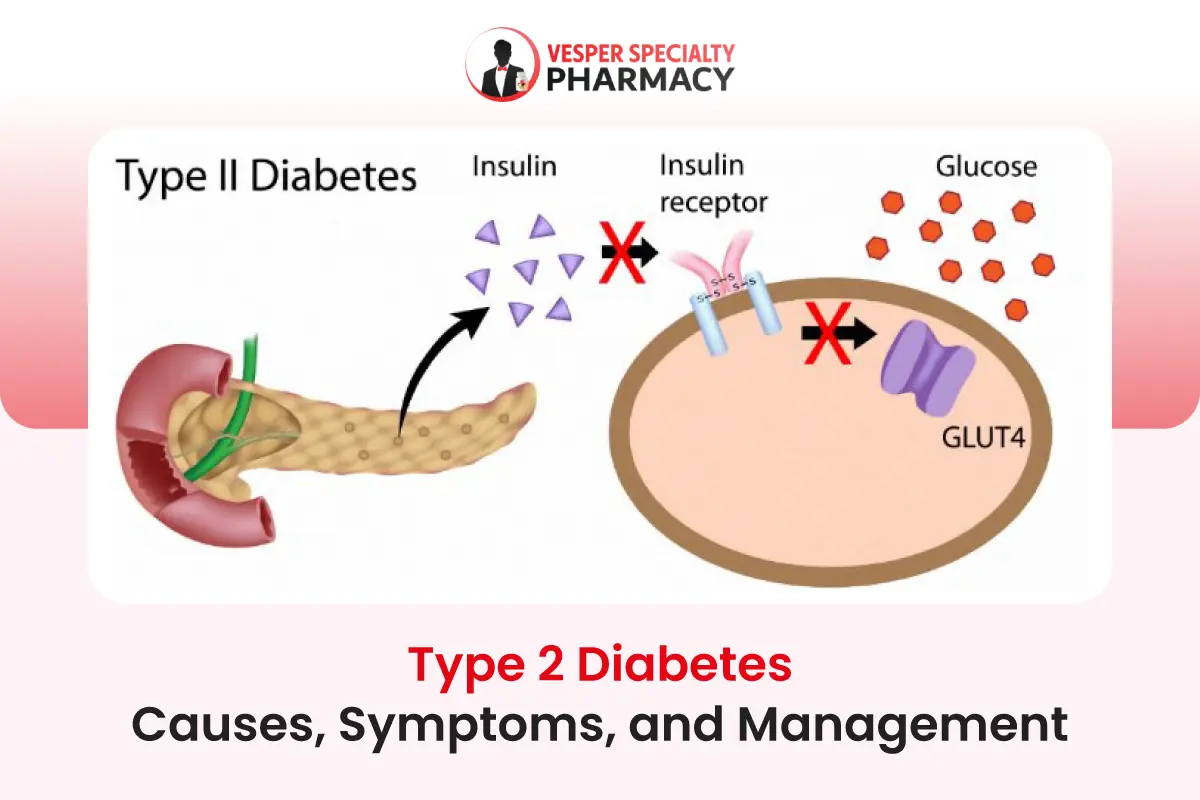
Definition and Distinction from Type 1 Diabetes
Type 2 diabetes is a chronic metabolic disorder characterized by elevated blood sugar levels resulting from insulin resistance and relative insulin deficiency. Insulin is a hormone produced by the pancreas that helps regulate blood sugar levels by facilitating the uptake of glucose into cells for energy.
In type 2 diabetes, the body’s cells become resistant to the effects of insulin, causing glucose to accumulate in the bloodstream. Unlike type 1 diabetes, where the immune system attacks and destroys the insulin-producing beta cells in the pancreas, type 2 diabetes is primarily driven by lifestyle factors such as poor diet, lack of exercise, and obesity.
While genetics also play a role in type 2 diabetes, it is often considered a preventable and manageable condition through lifestyle modifications and medications.
Statistics on Prevalence and Impact Globally
Type 2 diabetes has reached epidemic proportions worldwide, with its prevalence rising dramatically in recent decades. According to the International Diabetes Federation (IDF), approximately 463 million adults aged 20-79 were living with diabetes in 2019, and this number is expected to rise to 700 million by 2045 if current trends continue.
The impact of type 2 diabetes extends beyond individual health, placing a significant burden on healthcare systems and economies. It is a leading cause of complications such as cardiovascular disease, kidney failure, blindness, and lower limb amputations, resulting in increased healthcare costs and reduced productivity.
Risk Factors Associated with Type 2 Diabetes
Understanding these risk factors is essential for identifying individuals at higher risk and implementing preventive measures to reduce the incidence of type 2 diabetes.
By addressing modifiable risk factors such as diet, physical activity, and weight management, individuals can significantly lower their risk of developing this chronic condition. Several factors contribute to the development of type 2 diabetes, including:
- Obesity: Excess body weight, particularly abdominal obesity, increases the risk of insulin resistance and type 2 diabetes.
- Physical Inactivity: Lack of regular physical activity impairs insulin sensitivity and glucose metabolism, increasing the risk of diabetes.
- Unhealthy Diet: Diets high in refined carbohydrates, sugars, and saturated fats contribute to insulin resistance and obesity, predisposing individuals to type 2 diabetes.
- Family History: A family history of diabetes increases the risk of developing type 2 diabetes, suggesting a genetic predisposition.
- Age: The risk of type 2 diabetes increases with age, particularly after the age of 45.
- Ethnicity: Certain ethnic groups, including African Americans, Hispanics, Native Americans, and Asian Americans, are at higher risk of developing type 2 diabetes.
- Gestational Diabetes: Women who develop gestational diabetes during pregnancy have an increased risk of developing type 2 diabetes later in life.
Causes of Type 2 Diabetes
Understanding the complex interplay of these factors is essential for preventing and managing type 2 diabetes. By addressing modifiable risk factors such as diet, exercise, and weight management, individuals can reduce their risk of developing this chronic condition and improve their overall health and well-being.
Insulin Resistance and Its Role
Insulin resistance is a key underlying mechanism in the development of type 2 diabetes. Normally, insulin facilitates the uptake of glucose into cells, where it is used for energy production. However, in insulin resistance, the body’s cells become less responsive to the action of insulin, leading to impaired glucose uptake.
As a result, blood sugar levels remain elevated, prompting the pancreas to produce more insulin in an attempt to compensate. Over time, this increased demand on the pancreas can lead to insulin deficiency and the development of type 2 diabetes.
Genetic Predisposition
While lifestyle factors play a significant role in the development of type 2 diabetes, genetics also contribute to an individual’s risk. Certain genetic variations can affect insulin production, insulin sensitivity, and glucose metabolism, increasing susceptibility to type 2 diabetes.
Individuals with a family history of diabetes are at higher risk of developing the condition, indicating a genetic predisposition. However, genetics alone are not sufficient to cause type 2 diabetes, and environmental factors such as diet and exercise play a crucial role in determining disease risk.
Lifestyle Factors: Diet, Exercise, and Obesity
Diet, exercise, and obesity are major modifiable risk factors for type 2 diabetes. A diet high in refined carbohydrates, sugars, and saturated fats can contribute to insulin resistance and weight gain, increasing the risk of diabetes. Conversely, a diet rich in whole grains, fruits, vegetables, and lean proteins can help maintain healthy blood sugar levels and reduce the risk of diabetes.
Physical inactivity is also strongly associated with the development of type 2 diabetes. Regular exercise improves insulin sensitivity, helps control weight, and reduces the risk of diabetes. Conversely, a sedentary lifestyle increases the risk of obesity and insulin resistance, predisposing individuals to type 2 diabetes.
Obesity is a major risk factor for type 2 diabetes, particularly abdominal obesity. Excess fat tissue, especially around the abdomen, secretes inflammatory substances that promote insulin resistance and impair glucose metabolism. Losing weight through diet and exercise can improve insulin sensitivity and reduce the risk of developing type 2 diabetes.
Other Contributing Factors
In addition to insulin resistance, genetic predisposition, and lifestyle factors, other factors may contribute to the development of type 2 diabetes. These include:
- Age: The risk of type 2 diabetes increases with age, particularly after the age of 45.
- Ethnicity: Certain ethnic groups, including African Americans, Hispanics, Native Americans, and Asian Americans, are at higher risk of developing type 2 diabetes.
- Gestational Diabetes: Women who develop gestational diabetes during pregnancy have an increased risk of developing type 2 diabetes later in life.
Symptoms of Type 2 Diabetes
The signs and symptoms of type 2 diabetes, the importance of early detection, and the potential complications if left untreated underscores the importance of proactive management and regular medical care for individuals with this condition.
Common Signs and Symptoms
Type 2 diabetes often develops gradually, and some individuals may not experience noticeable symptoms initially. However, as the condition progresses, common signs and symptoms may include:
- Increased Thirst: Excessive thirst (polydipsia) is often one of the earliest symptoms of type 2 diabetes. High blood sugar levels cause dehydration, leading to increased thirst.
- Frequent Urination: Excess glucose in the bloodstream can overwhelm the kidneys’ ability to reabsorb it, leading to increased urination (polyuria).
- Fatigue: Despite adequate rest, individuals with type 2 diabetes may experience persistent fatigue and weakness due to the body’s inability to effectively utilize glucose for energy.
- Blurred Vision: High blood sugar levels can cause fluid to be pulled from the lenses of the eyes, leading to blurred vision and difficulty focusing.
- Slow Wound Healing: Type 2 diabetes can impair the body’s ability to heal wounds and injuries, increasing the risk of infections and complications.
- Recurrent Infections: Elevated blood sugar levels weaken the immune system, making individuals with type 2 diabetes more susceptible to infections, such as urinary tract infections, skin infections, and yeast infections.
- Unexplained Weight Loss: Despite increased appetite and food intake, some individuals with type 2 diabetes may experience unexplained weight loss due to the body’s inability to properly utilize glucose and breakdown fat for energy.
- Tingling or Numbness: Type 2 diabetes can damage nerves (diabetic neuropathy), leading to tingling, numbness, or pain, usually in the hands, feet, or legs.
Importance of Early Detection
Early detection of type 2 diabetes is crucial for preventing complications and improving outcomes. Many individuals with type 2 diabetes may not experience symptoms until the condition has progressed, making regular screening and blood sugar monitoring essential, especially for those at higher risk.
Early diagnosis allows for timely intervention and management strategies, including lifestyle modifications, medications, and blood sugar monitoring, to prevent or delay the progression of the disease and reduce the risk of complications.
Potential Complications if Left Untreated
If left untreated or poorly managed, type 2 diabetes can lead to serious complications affecting various organs and systems in the body. Some potential complications include:
- Cardiovascular Disease: Type 2 diabetes significantly increases the risk of heart disease, including heart attack, stroke, and peripheral artery disease.
- Nerve Damage (Neuropathy): Diabetes can damage the nerves throughout the body, leading to pain, numbness, tingling, and loss of sensation, particularly in the hands and feet.
- Kidney Disease (Nephropathy): Diabetes is a leading cause of kidney failure, known as diabetic nephropathy, which can require dialysis or kidney transplantation.
- Eye Damage (Retinopathy): High blood sugar levels can damage the blood vessels in the retina, leading to diabetic retinopathy, a leading cause of blindness in adults.
- Foot Complications: Diabetes can cause nerve damage and poor blood circulation in the feet, increasing the risk of foot ulcers, infections, and even amputation if not properly treated.
- Skin Conditions: Individuals with type 2 diabetes are at higher risk of developing skin conditions, such as bacterial and fungal infections, diabetic dermopathy, and acanthosis nigricans.
Diagnosis and Screening
Individuals with prediabetes, defined as impaired fasting glucose (IFG) or impaired glucose tolerance (IGT), should undergo annual screening for type 2 diabetes to monitor their risk and prevent progression to diabetes.
Screening for type 2 diabetes should be individualized based on risk factors, age, and other clinical considerations, with the goal of identifying those at risk and implementing appropriate interventions to prevent or manage the disease effectively.
Methods Used for Diagnosis
Diagnosing type 2 diabetes typically involves a combination of clinical evaluation, blood tests, and risk assessment. The following methods are commonly used for diagnosis:
- Fasting Plasma Glucose (FPG) Test: This test measures blood sugar levels after an overnight fast. A fasting blood glucose level of 126 milligrams per deciliter (mg/dL) or higher on two separate occasions indicates diabetes.
- Oral Glucose Tolerance Test (OGTT): This test involves fasting overnight followed by drinking a glucose solution. Blood sugar levels are measured before and two hours after consuming the solution. A blood glucose level of 200 mg/dL or higher two hours after drinking the glucose solution indicates diabetes.
- Hemoglobin A1c (HbA1c) Test: This test measures the average blood sugar level over the past two to three months. An HbA1c level of 6.5% or higher indicates diabetes.
- Random Plasma Glucose Test: This test measures blood sugar levels at any time of the day, regardless of when the individual last ate. A blood glucose level of 200 mg/dL or higher, along with symptoms of diabetes, indicates diabetes.
Importance of Regular Screening
Regular screening for type 2 diabetes is essential for early detection and prevention of complications. Many individuals with type 2 diabetes may not experience noticeable symptoms in the early stages of the disease, making routine screening critical for identifying those at risk.
Early detection allows for timely intervention and management strategies to prevent or delay the progression of the disease and reduce the risk of complications. It also provides an opportunity for individuals to make lifestyle modifications, such as adopting a healthy diet, increasing physical activity, and managing weight, to lower their risk of developing diabetes.
Who Should Get Screened and When
The American Diabetes Association (ADA) recommends the following screening guidelines for type 2 diabetes:
- Adults of Any Age: Adults of any age who are overweight or obese (body mass index [BMI] of 25 or higher) and have one or more additional risk factors for diabetes should be screened.
- Overweight Children and Adolescents: Overweight children and adolescents who have additional risk factors for diabetes should be screened annually, beginning at age 10 or at the onset of puberty.
- Adults Aged 45 and Older: Adults aged 45 and older should be screened for diabetes every three years, regardless of risk factors.
- Women with a History of Gestational Diabetes: Women who have a history of gestational diabetes should undergo screening for diabetes within six to 12 weeks after giving birth and then be screened every one to three years thereafter.
Management and Treatment Options
Managing type 2 diabetes involves a combination of lifestyle modifications, medications, and regular monitoring to control blood sugar levels and prevent complications. The following are common management and treatment options:
Lifestyle Modifications: Diet, Exercise, and Weight Management
Healthy Eating: Following a balanced diet that is rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help regulate blood sugar levels and maintain overall health. Limiting the intake of refined carbohydrates, sugars, and processed foods is also important.
Regular Exercise: Engaging in regular physical activity, such as brisk walking, cycling, swimming, or strength training, helps improve insulin sensitivity, lower blood sugar levels, and manage weight. Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week, along with muscle-strengthening activities on two or more days per week.
Weight Management: Losing excess weight, particularly abdominal fat, can significantly improve insulin sensitivity and glycemic control. Aim for gradual weight loss through a combination of dietary changes and increased physical activity, targeting a weight loss of 5-10% of body weight over six to 12 months.
Medications for Controlling Blood Sugar Levels
Oral Medications: Several classes of oral medications are available to lower blood sugar levels and improve insulin sensitivity, including metformin, sulfonylureas, meglitinides, thiazolidinediones, DPP-4 inhibitors, SGLT2 inhibitors, and GLP-1 receptor agonists. These medications may be used alone or in combination to achieve glycemic control.
Injectable Medications: For individuals who do not achieve adequate glycemic control with oral medications, injectable medications such as insulin and GLP-1 receptor agonists may be prescribed. These medications help lower blood sugar levels and may be used in combination with oral medications or as standalone therapies.
Insulin Therapy When Necessary
In some cases, insulin therapy may be necessary to achieve and maintain optimal blood sugar control. Insulin is typically used when oral medications and lifestyle modifications are insufficient to control blood sugar levels. Insulin therapy may involve multiple daily injections or the use of insulin pumps to deliver insulin continuously.
Importance of Regular Monitoring and Follow-ups
Regular monitoring of blood sugar levels, blood pressure, cholesterol levels, and kidney function is essential for individuals with type 2 diabetes to assess treatment effectiveness and detect any complications early. Self-monitoring of blood glucose using a glucometer or continuous glucose monitoring (CGM) system allows individuals to track their blood sugar levels and make adjustments to their treatment plan as needed.
Regular follow-up visits with healthcare providers, including primary care physicians, endocrinologists, diabetes educators, and dietitians, are important for ongoing management and support. These visits provide an opportunity to review treatment goals, adjust medications, address any concerns or challenges, and provide education and counseling on lifestyle modifications.
Complications of Type 2 Diabetes
Managing type 2 diabetes is crucial not only for controlling blood sugar levels but also for preventing or minimizing the risk of complications. This section explores both short-term and long-term complications associated with type 2 diabetes, as well as the importance of preventive measures and management strategies.
Short-term Complications: Hypoglycemia, Hyperglycemia
Hypoglycemia (Low Blood Sugar)
Hypoglycemia occurs when blood sugar levels drop too low, usually below 70 mg/dL. It can result from excessive insulin or certain diabetes medications, delayed or missed meals, excessive physical activity, or alcohol consumption.
Symptoms of hypoglycemia include shakiness, dizziness, sweating, confusion, irritability, and in severe cases, loss of consciousness or seizures. Prompt treatment with fast-acting carbohydrates such as glucose tablets, fruit juice, or candy can raise blood sugar levels and alleviate symptoms.
Hyperglycemia (High Blood Sugar)
Hyperglycemia occurs when blood sugar levels rise above the target range, typically above 180 mg/dL. It can result from inadequate insulin or diabetes medication, overeating, illness or infection, stress, or sedentary behavior.
Symptoms of hyperglycemia include increased thirst, frequent urination, fatigue, blurred vision, and slow wound healing. Long-term hyperglycemia can lead to complications such as cardiovascular disease, neuropathy, and retinopathy. Treatment involves adjusting insulin or medication doses, increasing physical activity, and monitoring blood sugar levels closely.
Long-term Complications: Cardiovascular Disease, Neuropathy, Retinopathy, Nephropathy
Cardiovascular Disease
Individuals with type 2 diabetes are at significantly higher risk of developing cardiovascular disease, including heart attack, stroke, and peripheral artery disease. High blood sugar levels, along with other risk factors such as high blood pressure, high cholesterol, and obesity, contribute to the development of atherosclerosis (hardening and narrowing of the arteries), increasing the risk of heart disease and stroke.
Neuropathy
Diabetes can damage the nerves throughout the body, leading to diabetic neuropathy. Symptoms may include numbness, tingling, burning sensations, or pain, usually in the hands, feet, or legs. Diabetic neuropathy can also affect digestive function, sexual function, and bladder control, leading to complications such as gastroparesis, erectile dysfunction, and urinary incontinence.
Retinopathy
Diabetes can damage the blood vessels in the retina (the light-sensitive tissue at the back of the eye), leading to diabetic retinopathy. Early stages may not cause noticeable symptoms, but as the condition progresses, it can cause vision loss and blindness. Regular eye exams and early intervention are essential for preventing or minimizing vision loss.
Nephropathy
Diabetes is a leading cause of kidney disease, known as diabetic nephropathy. High blood sugar levels and high blood pressure damage the kidneys’ filtering units (glomeruli), leading to proteinuria (excessive protein in the urine) and eventually kidney failure. Management involves blood sugar and blood pressure control, along with medications to protect kidney function.
Importance of Preventive Measures and Management
Preventing or minimizing the risk of complications is a key priority in managing type 2 diabetes. This includes:
- Achieving and maintaining optimal blood sugar control: Keeping blood sugar levels within the target range can help reduce the risk of both short-term and long-term complications.
- Managing blood pressure and cholesterol levels: Controlling high blood pressure and high cholesterol levels can reduce the risk of cardiovascular disease and kidney damage.
- Adopting a healthy lifestyle: Following a balanced diet, engaging in regular physical activity, maintaining a healthy weight, and avoiding tobacco use can help improve overall health and reduce the risk of complications.
- Regular medical care and monitoring: Regular check-ups, screenings, and monitoring of blood sugar levels, blood pressure, cholesterol levels, kidney function, and eye health are essential for early detection and management of complications.
Living with Type 2 Diabetes
Living with type 2 diabetes requires daily management and adaptation to maintain optimal health and well-being. This section discusses coping strategies, tips for managing the condition in daily life, and considerations for mental health.
Coping Strategies and Support Systems
- Education and Awareness: Learning about type 2 diabetes, its management, and potential complications can empower individuals to take control of their health. Attend diabetes education classes, join support groups, and stay informed about new developments in diabetes care.
- Seeking Support: Surround yourself with a supportive network of family, friends, healthcare providers, and fellow individuals with diabetes. Share your experiences, concerns, and successes with others who understand what you’re going through.
- Stress Management: Stress can affect blood sugar levels and overall health. Practice relaxation techniques such as deep breathing, meditation, yoga, or mindfulness to reduce stress and promote emotional well-being.
- Problem-Solving Skills: Develop problem-solving skills to address challenges and obstacles related to managing diabetes. Break down tasks into manageable steps, set realistic goals, and seek creative solutions to overcome barriers.
- Positive Outlook: Maintain a positive attitude and focus on what you can control. Celebrate small victories, stay optimistic about your ability to manage diabetes effectively, and practice self-compassion.
Tips for Managing the Condition in Daily Life
- Healthy Eating: Follow a balanced diet that includes a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. Monitor portion sizes, limit added sugars and refined carbohydrates, and aim for consistency in meal timing and composition.
- Regular Physical Activity: Incorporate regular exercise into your daily routine to improve insulin sensitivity, manage weight, and promote overall health. Choose activities you enjoy, such as walking, cycling, swimming, or dancing, and aim for at least 150 minutes of moderate-intensity exercise per week.
- Medication Adherence: Take your medications as prescribed by your healthcare provider and follow their instructions for monitoring blood sugar levels. Keep track of medications, refills, and appointments to ensure consistent management of diabetes.
- Blood Sugar Monitoring: Monitor your blood sugar levels regularly using a glucometer or continuous glucose monitoring (CGM) system. Keep a log of your readings and discuss them with your healthcare provider to make adjustments to your treatment plan as needed.
- Foot Care: Inspect your feet daily for any cuts, sores, blisters, or signs of infection. Keep your feet clean and moisturized, wear comfortable shoes that fit well, and avoid going barefoot to prevent foot complications.
Mental Health Considerations
- Emotional Support: Living with diabetes can be challenging emotionally. Seek support from loved ones, healthcare providers, or mental health professionals to cope with feelings of stress, anxiety, or depression.
- Self-Care: Prioritize self-care activities that promote mental and emotional well-being, such as engaging in hobbies, spending time with loved ones, practicing relaxation techniques, and getting enough sleep.
- Diabetes Distress: Recognize signs of diabetes distress, such as feelings of overwhelm, frustration, or burnout related to managing diabetes. Addressing these feelings through self-care, support, and professional help can improve overall quality of life.
- Stay Informed: Stay informed about the relationship between diabetes and mental health, and be proactive in addressing any concerns or challenges that arise. Educate yourself about strategies for managing stress, anxiety, or depression while living with diabetes.
Prevention of Type 2 Diabetes
Preventing type 2 diabetes is essential for reducing the burden of this chronic condition and improving public health outcomes. This section discusses the importance of preventive measures, strategies for reducing risk factors, and the role of public health initiatives and community support.
Importance of Preventive Measures
Health Impact: Type 2 diabetes is a significant public health concern worldwide, contributing to a range of complications and reducing quality of life. Preventing or delaying the onset of type 2 diabetes can improve overall health outcomes and reduce the risk of associated complications, such as cardiovascular disease, neuropathy, retinopathy, and nephropathy.
Cost Savings: Preventing type 2 diabetes can lead to substantial cost savings for healthcare systems and economies by reducing the need for medical interventions, medications, and hospitalizations associated with diabetes-related complications. Investing in prevention efforts can yield long-term benefits in terms of healthcare expenditures and productivity.
Quality of Life: Preventive measures not only reduce the risk of developing type 2 diabetes but also promote overall health and well-being. Adopting healthy lifestyle habits can improve energy levels, mood, and overall quality of life, leading to better physical and mental health outcomes.
Strategies for Reducing Risk Factors
Healthy Eating: Follow a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit intake of sugary beverages, processed foods, and high-calorie snacks. Choose nutrient-dense foods and practice portion control to maintain a healthy weight and prevent obesity.
Regular Physical Activity: Engage in regular physical activity to improve insulin sensitivity, lower blood sugar levels, and manage weight. Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week, along with muscle-strengthening activities on two or more days per week.
Weight Management: Maintain a healthy weight through a combination of diet, exercise, and lifestyle modifications. Aim for gradual weight loss if overweight or obese, targeting a weight loss of 5-10% of body weight over six to 12 months. Achieving and maintaining a healthy weight can reduce the risk of developing type 2 diabetes and its complications.
Smoking Cessation: Quit smoking or avoid tobacco use altogether. Smoking increases the risk of type 2 diabetes and complicates its management by impairing insulin sensitivity and increasing the risk of cardiovascular disease. Seek support from healthcare providers, quit-smoking programs, or support groups to quit smoking successfully.
Regular Screening: Individuals at higher risk of developing type 2 diabetes, such as those with a family history, overweight or obese individuals, and those with prediabetes, should undergo regular screening to detect diabetes early and implement preventive measures promptly. Screening may involve blood tests, such as fasting plasma glucose, oral glucose tolerance, or hemoglobin A1c tests, as recommended by healthcare providers.
Public Health Initiatives and Community Support
Health Education Programs: Public health initiatives aimed at raising awareness about type 2 diabetes risk factors, preventive measures, and healthy lifestyle habits can empower individuals to make informed choices about their health. Health education programs, workshops, and community outreach efforts can provide valuable information and resources to support prevention efforts.
Community Resources: Access to community resources, such as recreational facilities, parks, walking trails, farmers’ markets, and healthy food options, can promote physical activity and healthy eating habits. Collaborations between healthcare providers, community organizations, schools, workplaces, and local governments can create supportive environments that facilitate healthy behaviors and prevent type 2 diabetes.
Policy Changes: Policy changes at the local, state, and national levels can influence environmental factors that contribute to type 2 diabetes risk, such as access to healthy food options, opportunities for physical activity, and tobacco control measures. Advocating for policies that promote healthy lifestyles, reduce disparities, and improve access to preventive care can have a positive impact on population health and diabetes prevention efforts.
References
Citations for Statistics and Research Studies
Centers for Disease Control and Prevention. (2021). National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services.
American Diabetes Association. (2022). Standards of Medical Care in Diabetes—2022. Diabetes Care, 45(Supplement 1), S1–S234.
International Diabetes Federation. (2021). IDF Diabetes Atlas, 10th Edition. Brussels, Belgium: International Diabetes Federation.
Kahn, S. E., Cooper, M. E., & Del Prato, S. (2014). Pathophysiology and treatment of type 2 diabetes: Perspectives on the past, present, and future. The Lancet, 383(9922), 1068–1083.
Additional Resources for Further Reading
Diabetes Education Online. (n.d.). Retrieved from https://dtc.ucsf.edu/types-of-diabetes/type2/
National Institute of Diabetes and Digestive and Kidney Diseases. (2022). Type 2 Diabetes. Retrieved from https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/type-2-diabetes
Mayo Clinic. (2022). Type 2 Diabetes. Retrieved from https://www.mayoclinic.org/diseases-conditions/type-2-diabetes/symptoms-causes/syc-20351193
American Diabetes Association. (2022). Diabetes Food Hub. Retrieved from https://www.diabetesfoodhub.org/
Centers for Disease Control and Prevention. (2022). Preventing Type 2 Diabetes. Retrieved from https://www.cdc.gov/diabetes/prevention/index.html